3 signs your IBS may be IBD
I saw her three months ago.
Mid-thirties, exhausted, losing weight despite eating normally.
The grumbling abdominal pain was now constant.
Loose motions that were worsening.
“I’ve had IBS for years,” she told me. “This is just a bad flare.”
It wasn’t.
After some blood tests and a colonoscopy, we found Crohn’s disease.
Definitely NOT IBS.
Real inflammation, not just sensitivity.
She’s on treatment now and doing much better. Her energy returned and her weight came back. The pain (finally) settled.
That consultation made me think about how often this happens…how the line between IBS and IBD can blur, especially when symptoms worsen or change.
Let me explain some important differences
Two different conditions
IBS is very common. IBD not so common.
Irritable Bowel Syndrome (IBS) is a disorder of gut function, not structure or inflammation.
The stomach, small and large bowel looks perfect on endoscopy.
No visible damage. No inflammation markers. Just heightened sensitivity and altered motility patterns.
The gut-brain axis (the nerves that link your brain and digestive system) becomes dysregulated, creating visceral hypersensitivity. Your gut’s pain signalling system becomes overactive.
I’ve written about IBS before in Opening Your Mind to Irritable Bowel (I also talk about IBS symptoms and diagnosis). Visceral hypersensitivity affects 60-90% of patients with IBS.
The gut-brain axis communicates through neuronal, hormonal, and immune pathways. The pain is absolutely real. But there’s no structural abnormality causing it.
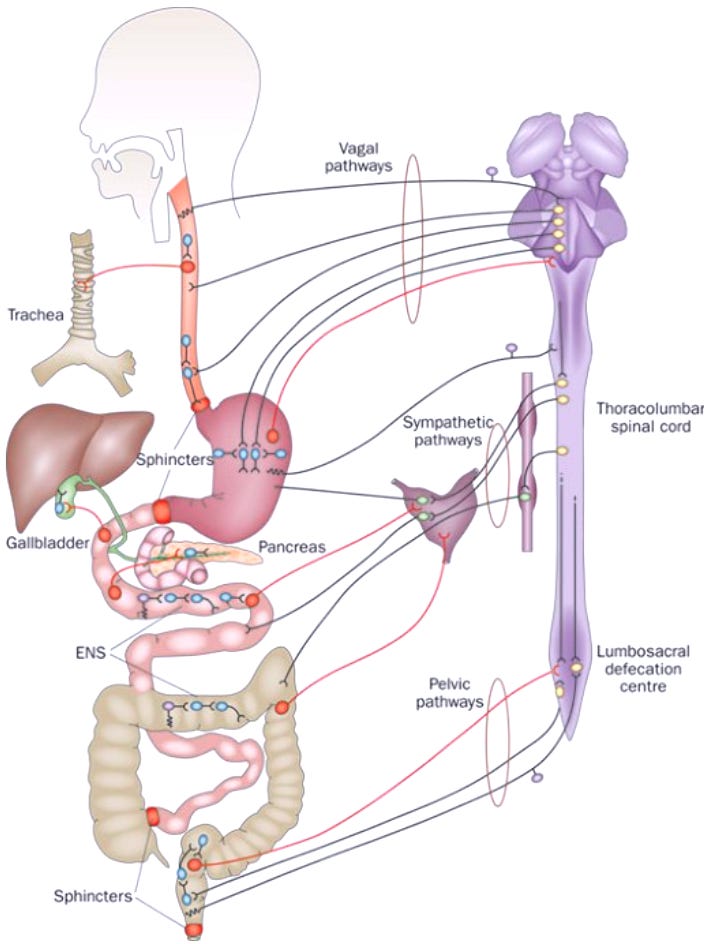
Your gut and brain are linked via the enteric nervous system….when it becomes overactive IBS develops!
Inflammatory Bowel Disease (IBD) is different entirely.
It’s autoimmune. Inflammatory. Systemic.
Your immune system mistakenly attacks healthy intestinal tissue, causing visible inflammation and damage.
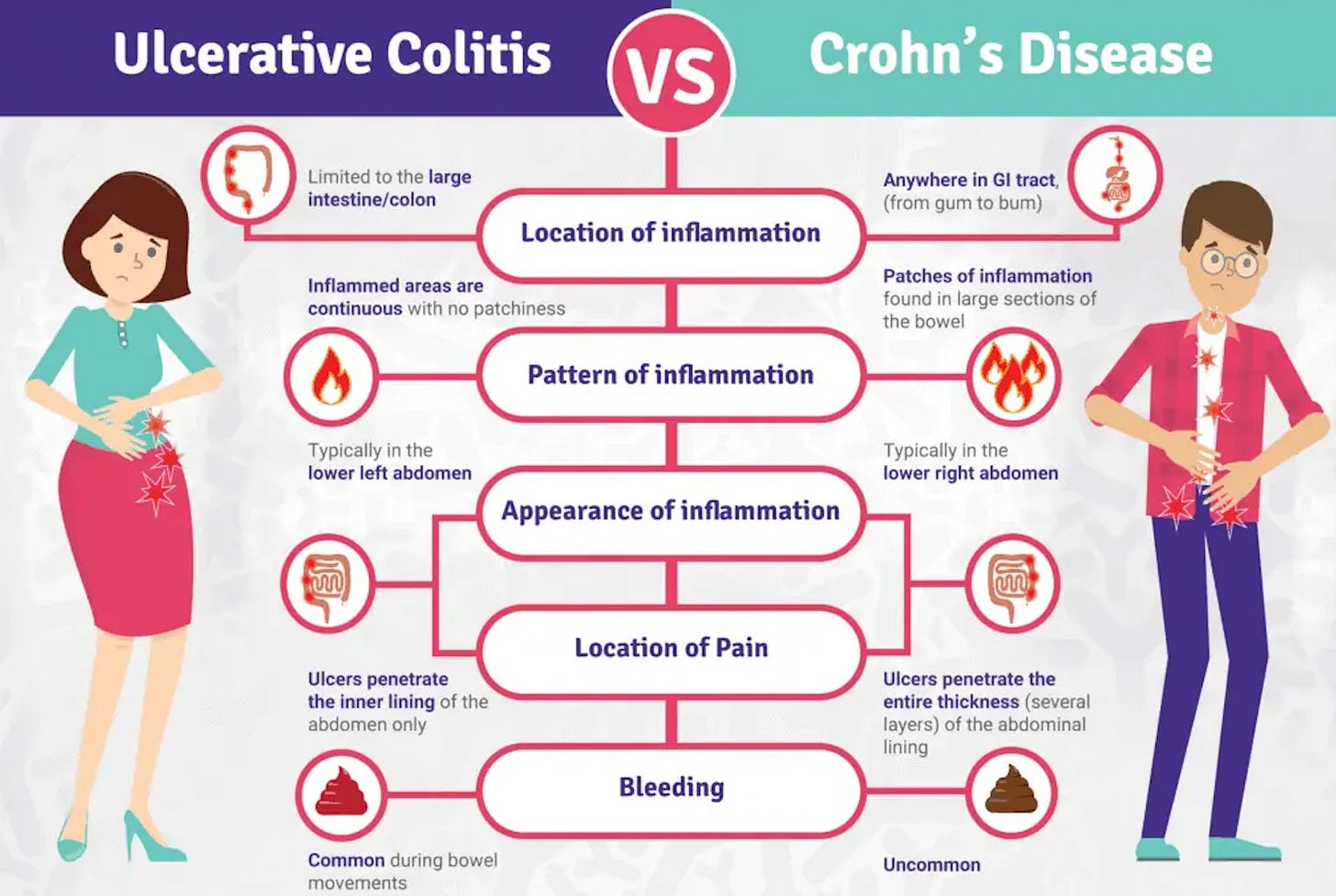
IBD is split into Crohn’s disease and ulcerative colitis; creating ulcers, erosions, and structural changes you can see on endoscopy and measure with inflammatory markers.
The inflammation doesn’t just stay in the gut; it spills over, affecting other organs.
Joints. Skin. Eyes.
https://occtopus.org.uk/insights/understanding-inflammatory-bowel-disease-ibd-a-comprehensive-guide/
So how do you tell the difference? Here are three key signs.
Join my newsletter….improving your liver and gut health…one e-mail at a time!
https://drhussenbux.substack.com/
Sign 1: Chronicity of symptoms
Diarrhoea lasting more than two weeks should always make you pause.
IBS can cause diarrhoea, yes.
But IBD brings a different pattern…
Persistent, unrelenting, progressive. The symptoms don’t come and go with stress or diet triggers. They accumulate. Build. Wear you down.
Weight loss without trying? That’s not typical for IBS. IBD causes malabsorption, reduces appetite through inflammatory cytokines (type of protein), and literally consumes energy fighting itself.
Studies show unintentional weight loss is an independent predictor of Crohn’s disease versus IBS.
Fatigue that won’t shift? Look deeper. IBD commonly causes anaemia, especially iron deficiency, in up to half of patients.
The mechanism? Chronic intestinal blood loss, decreased iron absorption, and inflammation-induced bone marrow suppression.
Your body basically can’t make enough red blood cells.
You’re exhausted because you’re literally running low on oxygen carriers.
Disclaimer!! IBS causes fatigue too….it’s exhausting living with chronic symptoms. But IBS does NOT cause anaemia. No objective inflammatory markers. No progressive deterioration.
NICE guidelines suggest symptoms lasting 4-6 weeks warrant IBD suspicion.
Japanese gastroenterology guidelines emphasise persistent or recurrent symptoms, particularly in younger patients.
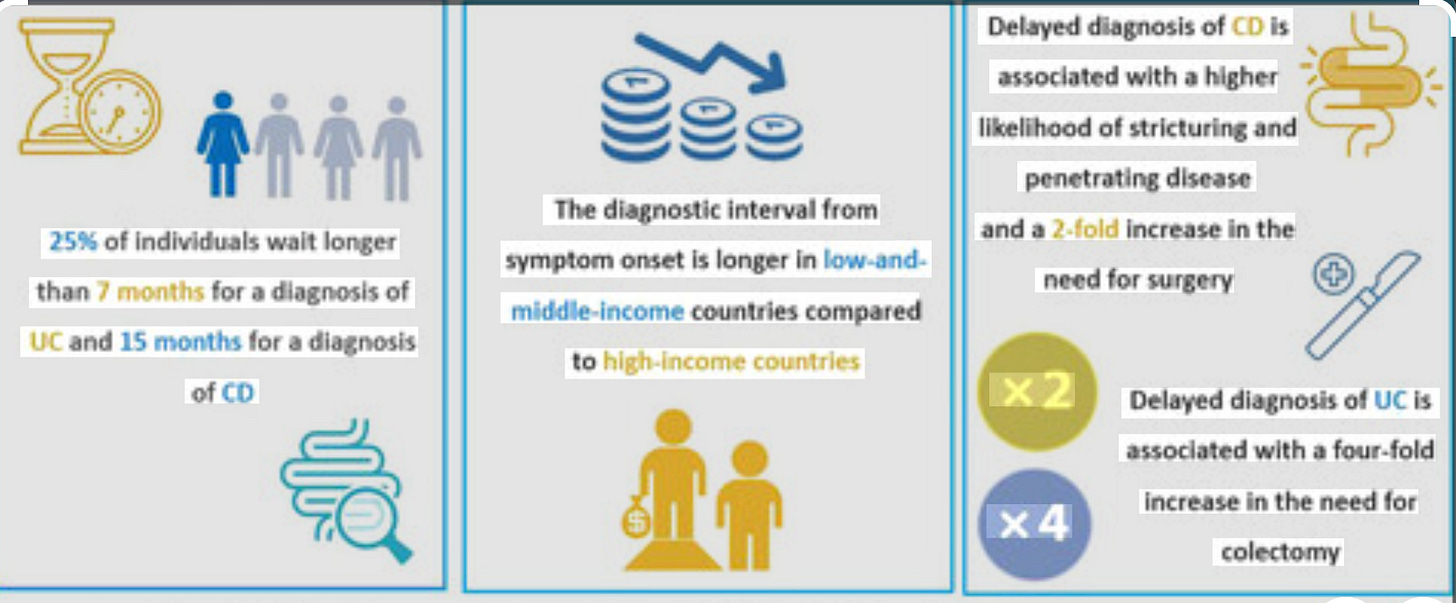
The diagnostic delay for IBD ranges from 2 months to 8 years; a delay associated with disease progression, complications, and increased surgery risk.
If your symptoms have shifted from manageable to relentless, from intermittent to constant, that chronicity deserves investigation.
https://onlinelibrary.wiley.com/doi/10.1111/apt.17370
Sign 2: Extra-intestinal manifestations
extra-intesta what??? Stay with me here!
This is a fancy way of saying inflammatory changes OUTSIDE of the gut.
Such as….
Mouth ulcers that appear with gut flares. Painful, recurrent aphthous ulcers affecting 4-20% of IBD patients, typically during active disease.

not fun
Rashes that coincide with diarrhoea.
Erythema nodosum – tender red nodules on the shins.
Pyoderma gangrenosum – painful ulcerating skin lesions.
These occur in 15-20% of IBD patients.

pyoderm gangrenosum
Joint pain or swelling with intestinal symptoms. Arthritis affects up to a third of IBD patients…knees, ankles, wrists, elbows become inflamed, often paralleling gut disease activity. Some develop axial arthritis, affecting the spine itself.
Why does this happen? Intestinal bacteria share space with tissues in joints, skin, and other organs. When the intestinal barrier becomes leaky, which happens in IBD, bacteria translocate across. The adaptive immune response can’t distinguish between bacterial epitopes and self-tissue.
It attacks both. Add systemic inflammatory cytokines circulating from the inflamed gut, and you get inflammation at distant sites.
This is the key difference. IBS does NOT cause extra-intestinal manifestations.
The symptoms stay confined to gut function; pain, bloating, altered bowel habits. No rashes. No joint destruction. No mouth ulcers tied to bowel symptoms.
If your gut symptoms come packaged with other organ involvement, that’s not IBS. That’s systemic disease requiring further investigation.
Up to 50% of IBD patients develop extra-intestinal manifestations during their disease course; it’s common, significant, and diagnostic.
Sign 3: Bleeding in stools
Let me be direct: blood mixed with stools is NOT an IBS feature.
IBS involves functional disturbance without mucosal damage. No inflammation means no bleeding. If you have diagnosed IBS and start seeing blood, that’s a new problem requiring investigation. Always.
IBD patterns differ. Ulcerative colitis typically causes rectal bleeding; blood mixed with stool, often with mucus. It’s a majority feature.
Crohn’s disease often presents with non-bloody diarrhoea. But if combined with persistent pain, weight loss and chronicity (see point 1) you need investigations.
When someone presents with bloody diarrhoea, I start methodically.
First, stool cultures. Rule out infections….C. difficile, Salmonella, Shigella, Campylobacter. Infectious colitis mimics IBD perfectly in the acute phase.
ACG guidelines strongly recommend stool testing before diagnosing ulcerative colitis. Can’t treat properly without excluding infection.
If cultures are negative and bleeding persists, endoscopic evaluation is needed.
If I am not sure between IBS I may request a faecal calprotectin.
This test measures neutrophil-derived proteins in stool, a marker of intestinal inflammation. If abnormal, you guessed it…endoscopic evaluation is needed!
The cutoff values:
- Less than 50 mcg/g: Not suggestive of inflammation. IBD likelihood under 1%.
- 50-150 mcg/g: Borderline. Could be mild inflammation or NSAID use.
- Above 150 mcg/g: Suggestive of active inflammatory process.
Faecal calprotectin has a high negative predictive value.
In english, If it’s low and clinical assessment is reassuring, IBD is incredibly unlikely.
If it’s elevated….colonoscopy time!
Ileocolonoscopy with segmental biopsies to see what’s actually happening in the mucosa.
Rectal bleeding is a red flag in all major guidelines. NICE, ACG, Japanese Society of Gastroenterology. It warrants specialist referral and investigation. Not something to watch and wait on indefinitely.
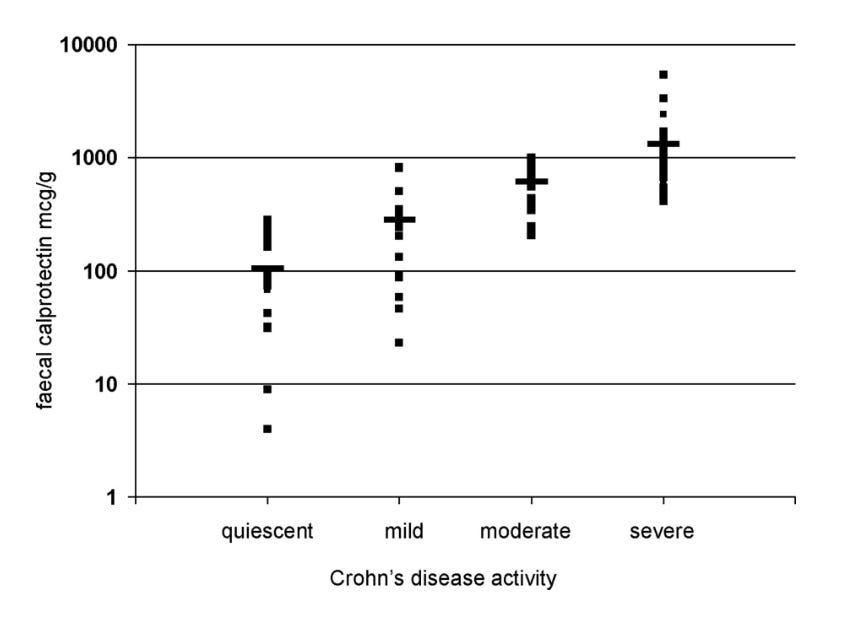
Faecal calprotectin levels plotted against Crohn’s disease activity (Dr James Turvill, Frontline Gastroenterology 2014)
IBS and IBD…..TOTALLY different diagnoses
IBS and IBD are fundamentally different conditions requiring different approaches.
IBS: functional disorder, visceral hypersensitivity, normal investigations, confined to gut symptoms, managed with diet, lifestyle, and medications targeting gut-brain axis.
IBD: autoimmune inflammatory disease, structural damage, systemic manifestations, requires immunosuppression or biologics targeting inflammation pathways.
If your “IBS” has become chronic and unrelenting, if you’re developing symptoms beyond the gut, if you’re seeing blood….these aren’t normal IBS variations. They’re signals to investigate further.
That patient I saw three months ago? Her life changed with proper diagnosis. The right treatment made all the difference. She stopped blaming herself for not managing her “IBS” better. She stopped restricting her diet endlessly. She started treating the real problem.
Diagnostic delay in IBD associates with worse outcomes; more complications, more surgery, more disability.
If something feels different, if your gut instinct says this isn’t right….listen to it!!
Seek specialist assessment. Get proper investigation. The difference between IBS and IBD may not always be obvious, but looking for these three signs: chronicity with systemic features, extra-intestinal manifestations, rectal bleeding, can guide you toward the right diagnosis.
Struggling with liver or gut issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
Struggling with liver or gut issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References:
Black CJ, et al. Efficacy of a low FODMAP diet in irritable bowel syndrome: systematic review and network meta-analysis. Gut 2021;70:1110-1116.
Dajti E, et al. Fecal calprotectin in differentiating IBD from IBS: systematic review and meta-analysis of 17 studies. Multiple sources 2020-2023.
Japanese Society of Gastroenterology. Evidence-based Clinical Practice Guidelines for Inflammatory Bowel Disease 2020. J Gastroenterol 2020;55:635-653. PMC8137635.
Mayo Clinic Laboratories. Fecal Calprotectin, Stool. Test interpretation guidelines 2024.
National Institute for Health and Care Excellence (NICE). Inflammatory bowel disease Quality Standard [QS81]. Published 2015, updated 2024.
National Institute for Health and Care Excellence (NICE). Faecal calprotectin diagnostic tests for inflammatory diseases of the bowel [DG11]. Published 2013.
Petryszyn P, et al. Fecal calprotectin in the diagnosis of inflammatory bowel disease: meta-analysis of 5,032 patients. Multiple systematic reviews 2018-2023.
Rubin DT, et al. ACG Clinical Guideline: Ulcerative Colitis in Adults. Am J Gastroenterol 2019;114:384-413.
Saha L. Irritable bowel syndrome: pathogenesis, diagnosis, treatment, and evidence-based medicine. World J Gastroenterol 2014;20(22):6759-6773. PMC4051916.
Simren M, et al. Gut-brain axis mechanisms in irritable bowel syndrome. Nat Rev Gastroenterol Hepatol 2023;20:307-322.
Vavricka SR, et al. Extraintestinal manifestations of inflammatory bowel disease. Am J Gastroenterol 2011;106:110-119.
Zhu Y, et al. Systematic review with meta-analysis: Fecal calprotectin for differentiating inflammatory bowel disease from IBS. Multiple sources 2020-2024.
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.

