Your one stop guide to GLP-1s
I’ve been avoiding this topic.
Everyone and their dog has written about Ozempic, Wegovy, Mounjaro….the whole GLP-1 family.
Social media is saturated with celebrity transformations, miracle weight-loss stories, and heated debates about who “deserves” these medications.
The discourse has become exhausting. Who do you even trust??
After years of sitting across from patients struggling with obesity….watching them try every diet, every exercise program, every promise of lasting change….I couldn’t stay silent.
The science behind these medications represents something genuinely transformative.
Not perfect. Not without concerns. But transformative nonetheless.
So here are my thoughts on GLP-1 receptor agonists from a gastroenterologist’s perspective. The mechanisms, the evidence, the side effects (yes, we need to talk about those), and what happens when people stop taking them.
From someone who has prescribed them to my patients AND monitor them in even more people.
General disclaimer: These are just my thoughts. NOT my recommendations. If you are thinking of starting a GLP-1 medication speak to a professional first. GLP-1 receptor agonists require prescription and medical supervision. I have NO affiliations with any pharmaceutical company who manufacture/market GLP1 medications.
The obesity epidemic we’re facing
In the United States, 40% of adults now live with obesity. Insane….
Severe obesity (BMI over 40) affects almost 10% of the population, up from 5% just two decades ago.
Globally, obesity has more than doubled since 1990, affecting 890 million adults worldwide.
Behind each statistic is someone navigating a complex interplay of genetics, environment, metabolism, and psychology. Someone dealing with real health consequences.
Because obesity isn’t merely about appearance or weight.
It’s a chronic disease that fundamentally alters physiology.
Twenty-five percent of US adults have metabolic syndrome; that constellation of abdominal obesity, high blood pressure, elevated blood sugar, abnormal cholesterol.
The risk of developing type 2 diabetes increases exponentially.
Cardiovascular disease risk compounds.
The odds of developing knee osteoarthritis increase nearly sevenfold with severe obesity.
Cancer risk rises across multiple sites: endometrial, pancreatic, kidney, postmenopausal breast.
The mechanisms are complex….chronic low-grade inflammation, insulin resistance, hormonal dysregulation, mechanical stress on joints. And the cycle perpetuates itself. Obesity makes movement harder, which reduces activity, which worsens obesity. Inflammation begets more inflammation. Insulin resistance deepens.
For decades, we’ve told people the solution is simple. Eat less, move more.
If only it were that simple.
(P.S. IF you do want to read about the foods I avoid click here )
(P.P.S and the foods I DO eat here)
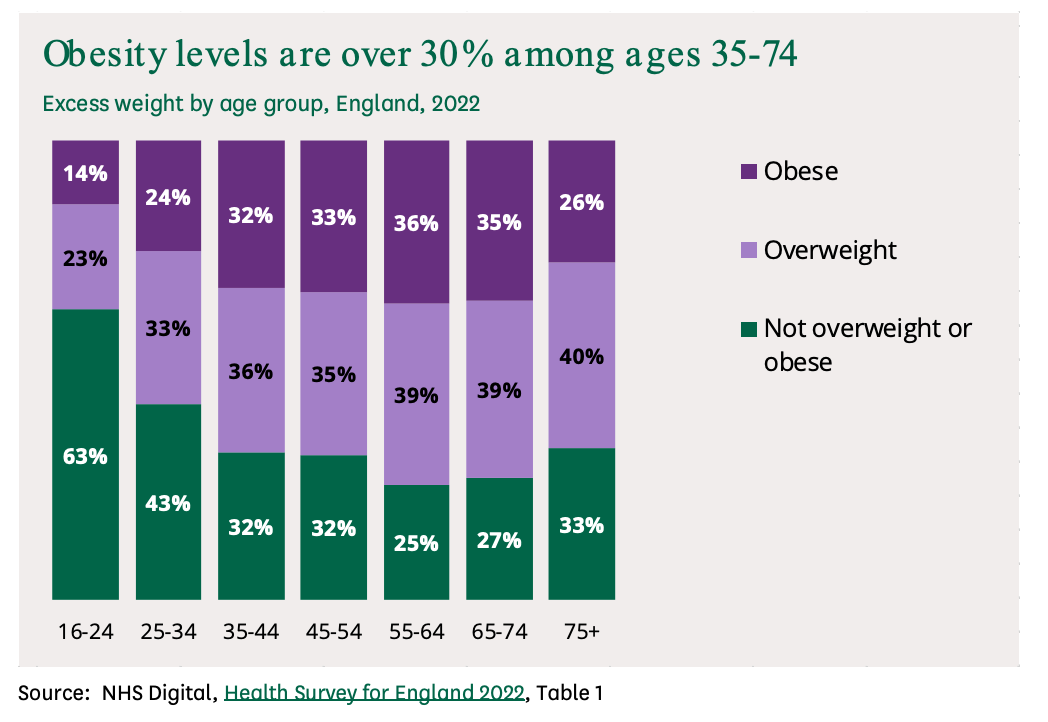
Here are the stats in England….almost as bad!
What we had before GLP-1s
The data on lifestyle interventions is….kind of how I expected it to be
Only about 20% of people with obesity achieve sustained weight loss of 10% or more through diet and exercise alone.
The average long-term weight loss with intensive lifestyle programs?
Around 5-10% of initial body weight after two years. And maintaining even that requires ongoing vigilance….300 minutes per week of physical activity, constant dietary monitoring, unwavering motivation.
Can you imagine how far a “lose weight with exercise and improved diet” speech goes during a 30 minute consultation?? I like to think it makes an impact but in reality it likely achieves little.
Tough stuff.
The Swedish Obese Subjects study followed over 2,000 people receiving conventional weight-loss treatment at 480 Swedish primary care centres.
After 10 years, 83% reported weight-loss attempts at every single follow-up.
Yet the average weight change?
An increase of 2%!!!!!!!! What the heck???
Only 12.5% achieved 10% weight loss, while 22% gained at least 10%.
SO how did this even happen??
When you lose weight, metabolic rate drops beyond what you’d predict from the reduction in body mass alone. Hunger hormones surge. The body defends its set point. These adaptations persist for years; in some cases up to six years after weight loss.
Bariatric surgery changed the conversation.
The Swedish Obese Subjects trial (the gold standard) demonstrated that gastric bypass and sleeve gastrectomy produced 17-23% sustained weight loss over 10-20 years.
Not 5%. Not 10%. Nearly a quarter of body weight, maintained for decades.
The surgery group had 30% lower mortality risk, 72% diabetes remission rates at two years, and substantial reductions in cardiovascular events.
Back of the net!!
The STAMPEDE trial showed that at five years, 29% of gastric bypass patients and 23% of sleeve gastrectomy patients achieved normal glucose levels without any diabetes medications. Compare that to 5% with intensive medical therapy alone.
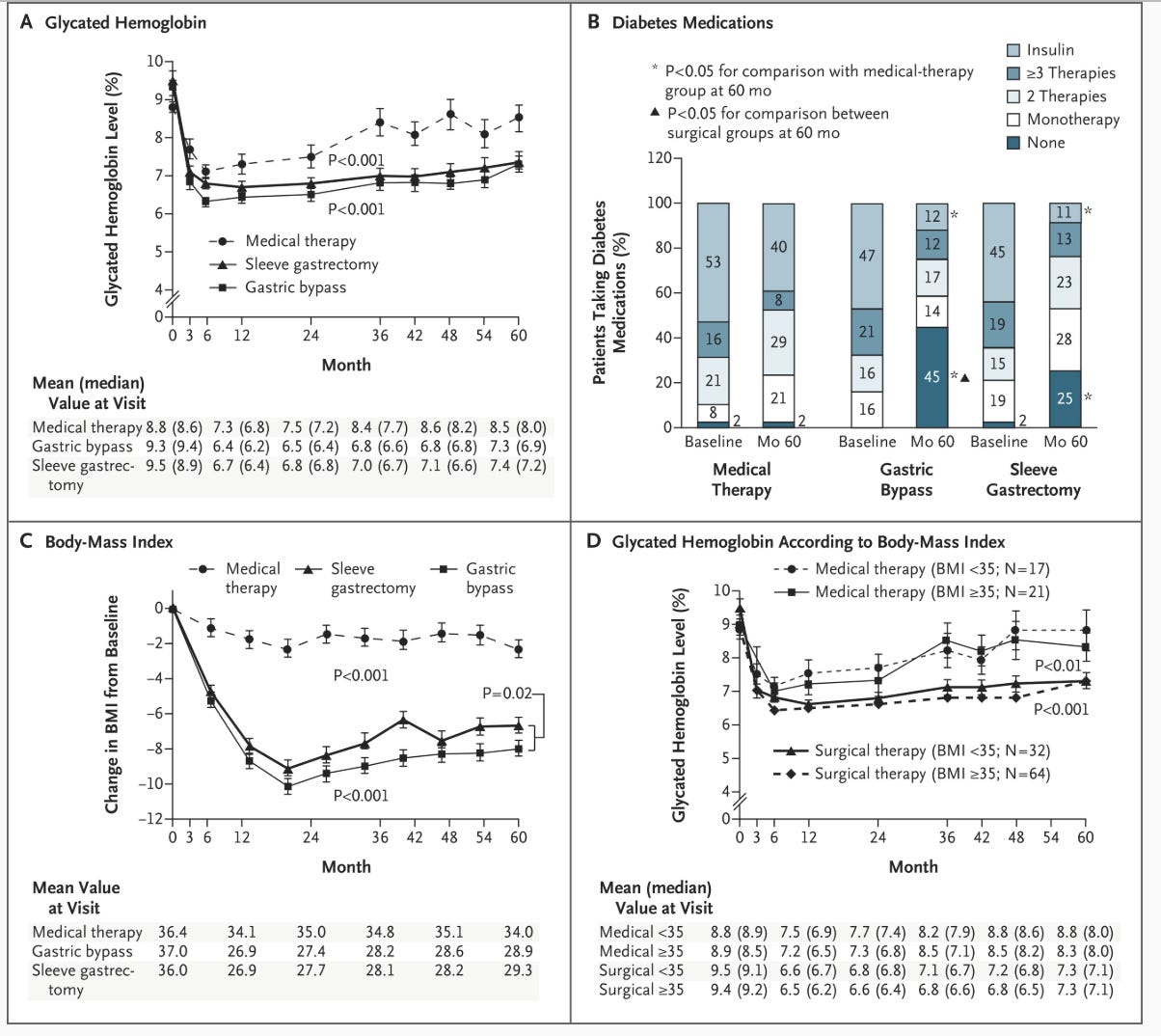
Bariatric surgery…….works
Bariatric surgery works. But it’s surgery. It carries risks; peri-operative mortality under 0.5%, complications in 2-5%, lifelong nutritional deficiencies requiring supplementation. And access remains limited by cost, insurance coverage, surgical capacity.
We needed something between “eat less, move more” and “rearrange your anatomy.”
Here come the GLP-1s!
OK so how do GLP-1s actually work?
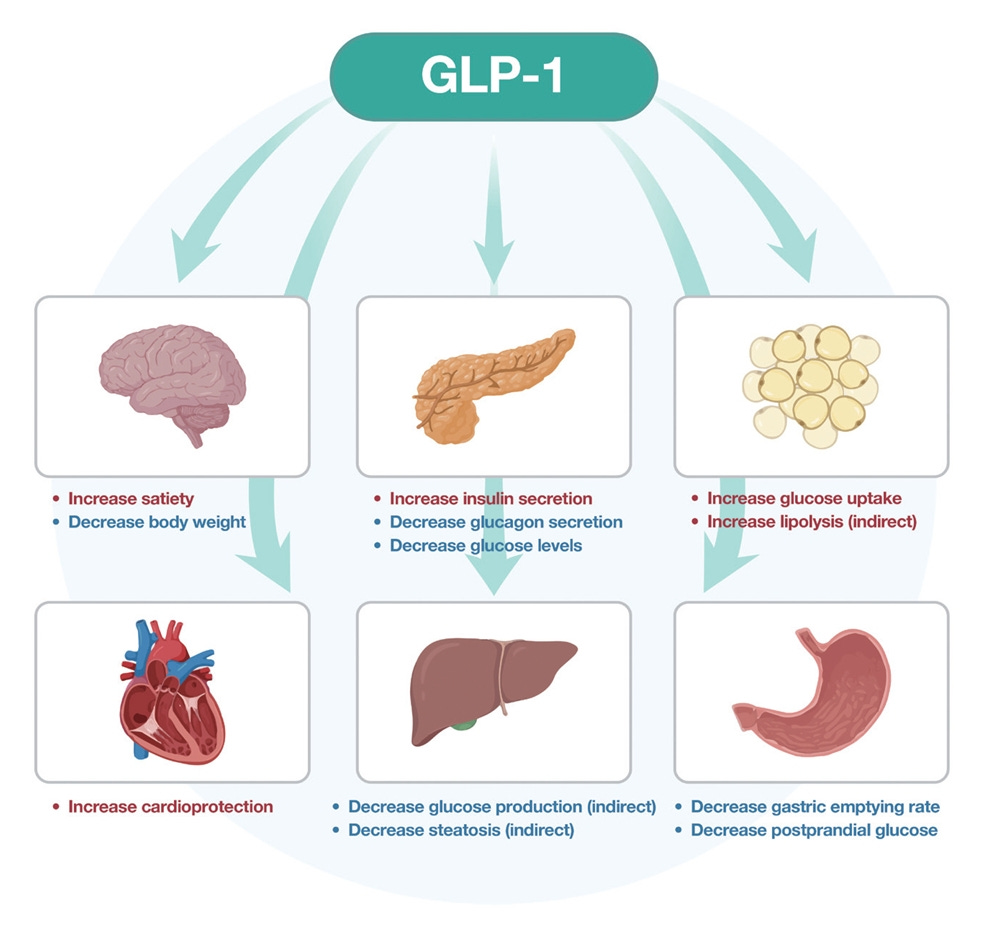
GLP-1 (glucagon-like peptide-1) is a hormone your gut produces naturally after you eat. Its job? Tell your brain you’re full, stimulate insulin release when blood sugar rises, slow gastric emptying, suppress glucagon secretion.
The problem is your body breaks down natural GLP-1 within 1-2 minutes.
GLP-1 receptor agonists solve this.
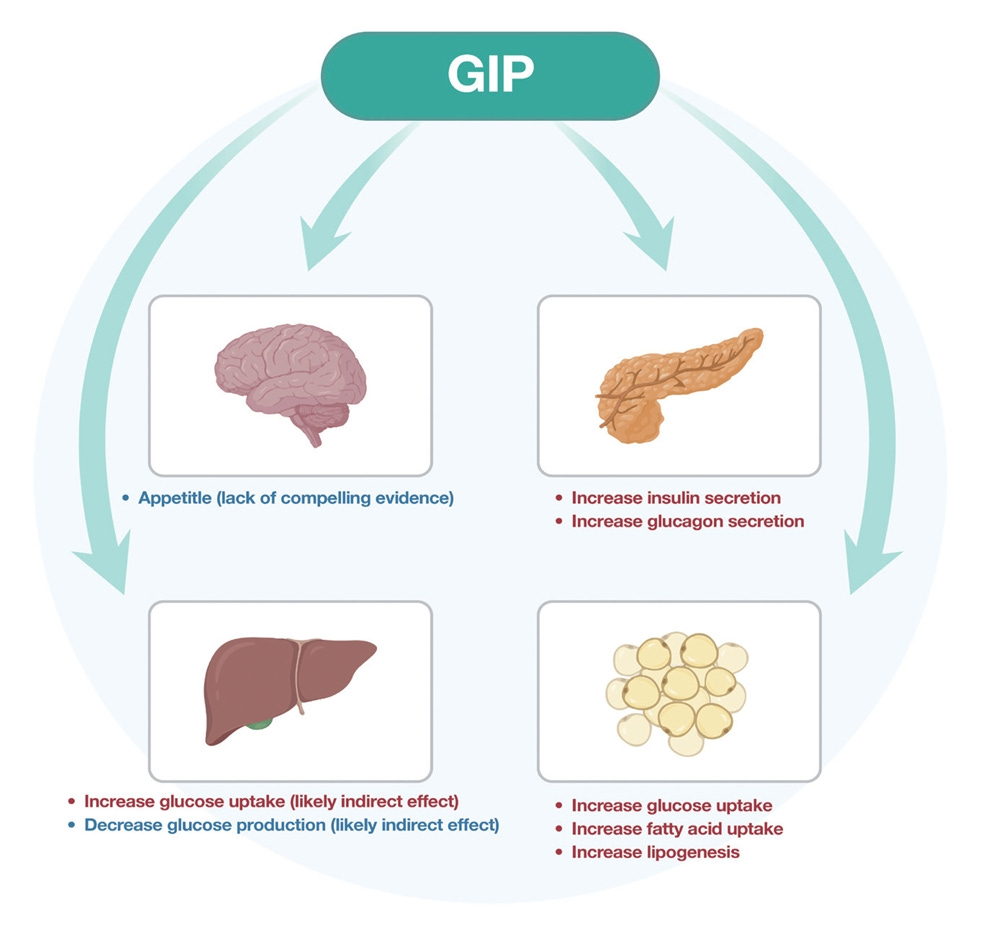
Semaglutide, liraglutide, tirzepatide (which actually targets both GLP-1 and GIP receptors)….these medications resist rapid breakdown.
They stick around. They activate GLP-1 receptors in the pancreas, the gut, and critically, the brain.
The weight loss happens primarily through the brain.
GLP-1 receptors in the hypothalamus region control appetite, satiety, food reward.
When GLP-1 receptor agonists bind there, they reset your body’s weight set point. They reduce hunger. They decrease food cravings. They change the psychological drive to eat.
https://e-enm.org/journal/view.php?doi=10.3803/EnM.2024.1942
And the landmark trials proved it works in humans.
STEP 1 enrolled 1,961 adults with obesity but without diabetes. After 68 weeks of semaglutide 2.4 mg weekly, participants lost an average of 15% of body weight compared to 2.4% with placebo.
Boom!
Eighty-six percent achieved at least 5% weight loss. Half lost more than 15%. One-third lost over 20%.
STEP 5 extended follow-up to two years. The weight loss persisted: 15.2% at 104 weeks.
SURMOUNT-1 tested tirzepatide – the dual GIP/GLP-1 receptor agonist. At the highest dose (15 mg weekly), average weight loss reached 22.5%. More than half of participants lost at least 20% of their body weight. Over a third lost 25% or more.
Let me repeat that: with tirzepatide, one-third of participants lost a quarter of their body weight.
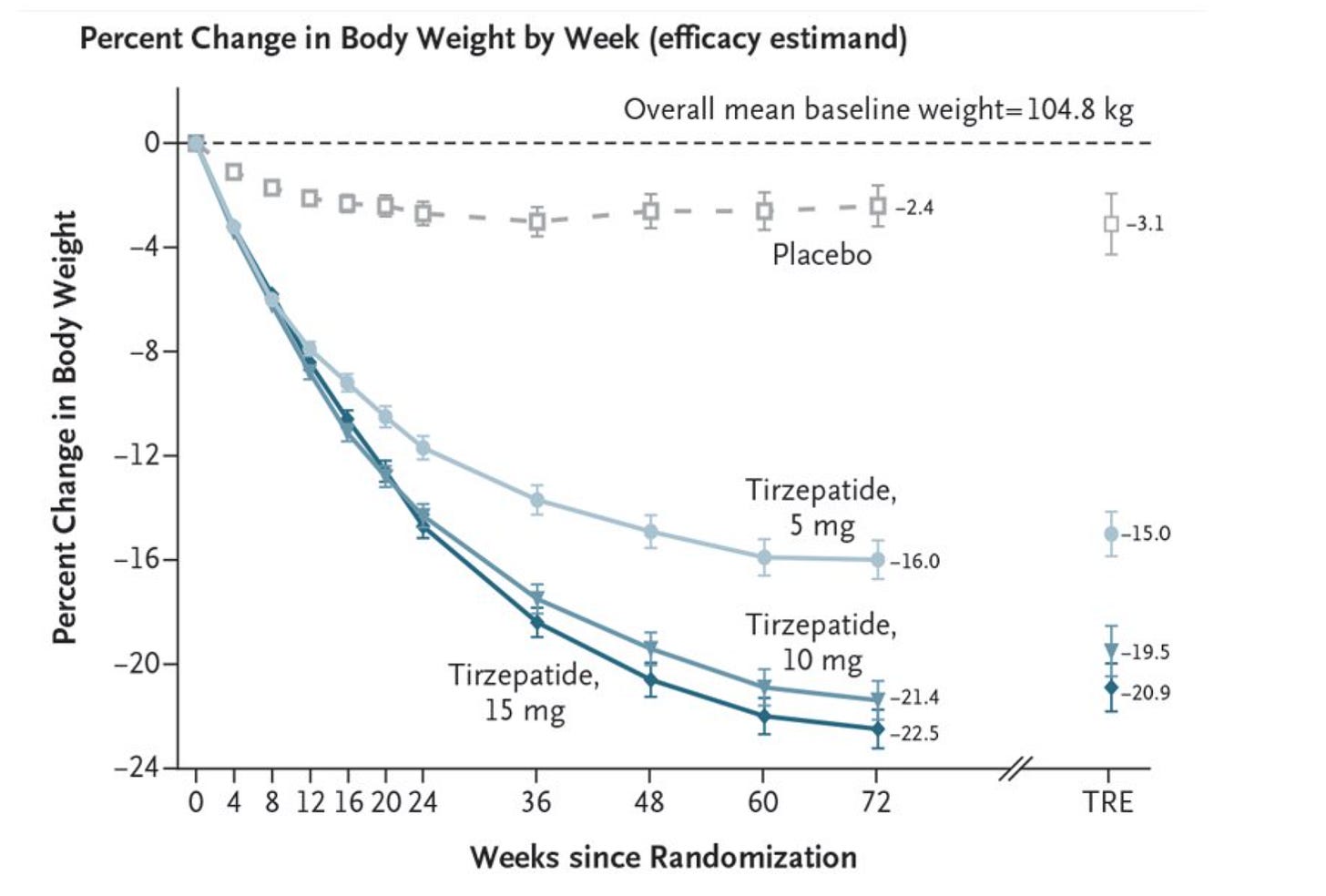
wowzer! https://www.nejm.org/doi/full/10.1056/NEJMoa2206038
These are weight reductions that approach bariatric surgery outcomes. With a weekly injection instead of an operation.
SUSTAIN-6 showed that semaglutide reduced major adverse cardiovascular events by 26%; primarily through a 39% reduction in stroke risk.
The SELECT trial in non-diabetic patients with cardiovascular disease demonstrated a 20% reduction in heart attacks and strokes.
Any side effects?
Well of course….there’s rarely a free win here!
Between 40-82% of people experience gastrointestinal symptoms.
Nausea is the most common, affecting 13-18% in most studies, often during dose escalation.
Diarrhoea occurs in 19-26%. Constipation in 8-17%.
For most people, these effects are mild-to-moderate and transient. They improve after a few weeks.
But for some, they’re intolerable. Discontinuation rates due to GI side effects run around 4-8%.
Rapid weight loss releases cholesterol into bile ducts, and GLP-1s may inhibit gallbladder motility. Therefore gallstone rates increase; in one real-world study of diabetic patients, 31% developed gallstones, and 60% of those became symptomatic.
It’s a bariatric surgery complication too….any rapid weight loss carries this risk.
Gastroparesis – delayed stomach emptying; initially generated alarming headlines. A 2023 study suggested nearly four times higher risk. But when researchers controlled for BMI (because obesity itself delays gastric emptying), the risk dropped to 2.3-fold, and disappeared entirely in people without diabetes.
Still worth monitoring. Still requires caution with certain surgeries and procedures. But the magnitude isn’t what initial reports suggested.
Pancreatitis remains controversial. Some early studies showed increased risk. But the largest, most rigorous analyses. including registry data from Scandinavia and propensity-matched US studies, show minimal to no increased risk.
Among patients without diabetes or prior pancreatitis, five-year data showed lower pancreatitis rates on GLP-1s (0.3% vs 0.4%). The medications may even be protective in the right populations.
Thyroid concerns arose from animal studies showing medullary thyroid cancer in rodents.
But human thyroid C-cells express GLP-1 receptors very differently.
The LEADER trial followed patients for 3-5 years and found no effect on calcitonin levels and no new thyroid cancers.
A Scandinavian study of 145,000 GLP-1 users showed no increased thyroid cancer risk. One French study suggested possible association, but the cardiovascular outcome trials, the highest-quality evidence show no signal.
There’s a black box warning against use in people with personal or family history of medullary thyroid cancer or multiple endocrine neoplasia type 2. That’s appropriate caution. But the human risk appears vastly lower than rodent models suggested.
One concern that’s genuine: muscle loss.
About 40% of weight reduction comes from lean body mass.
The SUSTAIN 8 study showed lean mass decreased 2.3 kg alongside total weight loss of 5.3 kg.
Sarcopenia – loss of muscle mass and strength is seen particularly in older adults. Resistance exercise and adequate protein intake are essential.
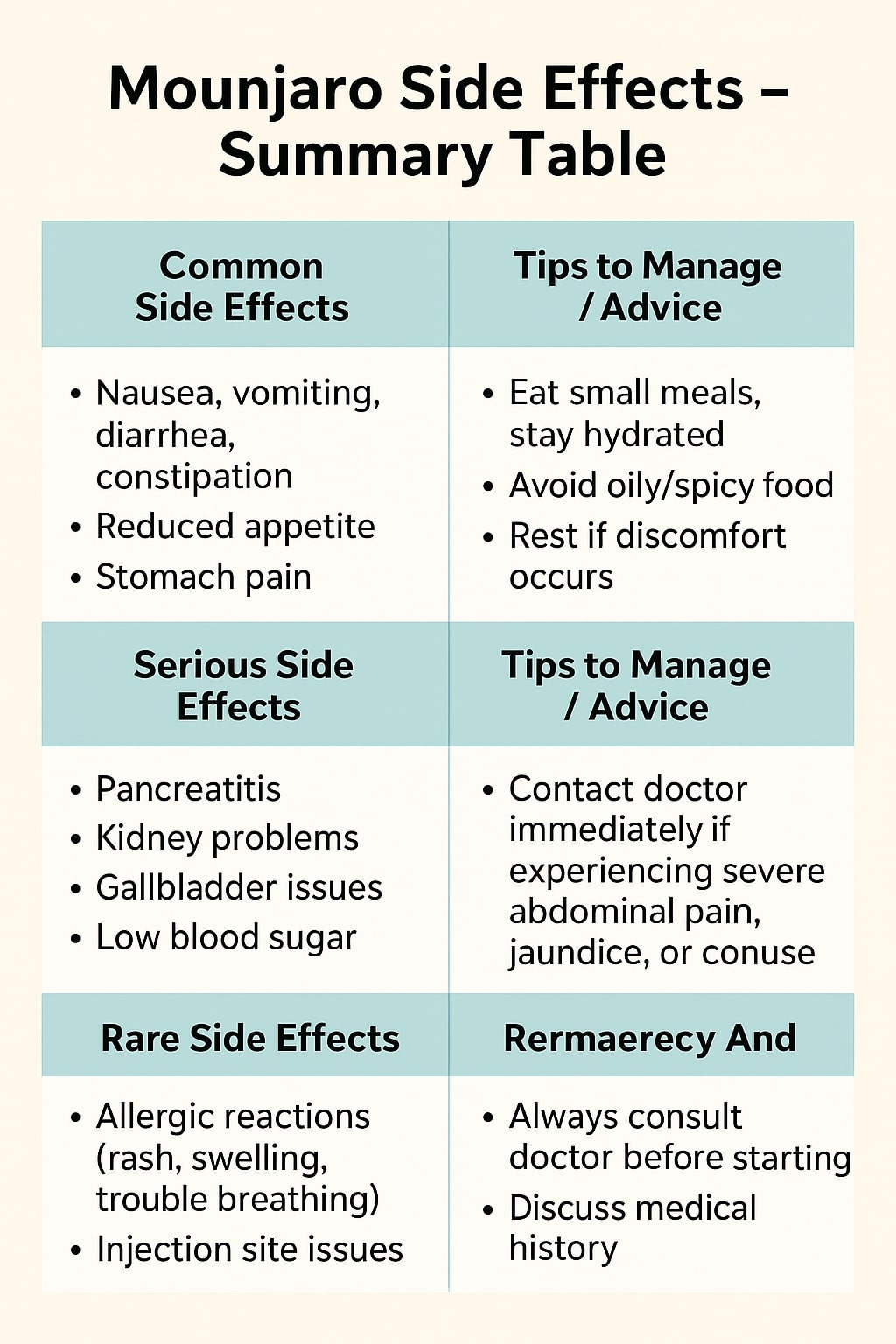
https://www.drrajatgoel.com/mounjaro-side-effects/
What happens when you stop???
This is the part that changes the conversation entirely.
STEP 4 randomised people who’d lost 10.6% on semaglutide to either continue the medication or switch to placebo.
Both groups maintained lifestyle interventions – 500-calorie daily deficit, 150 minutes weekly of physical activity.
The continuation group? They lost more weight, reaching 17.4% total reduction by week 68.
The placebo group? They regained 7% within 48 weeks.
Despite the lifestyle program. Despite their initial success. Despite doing “all the right things.”
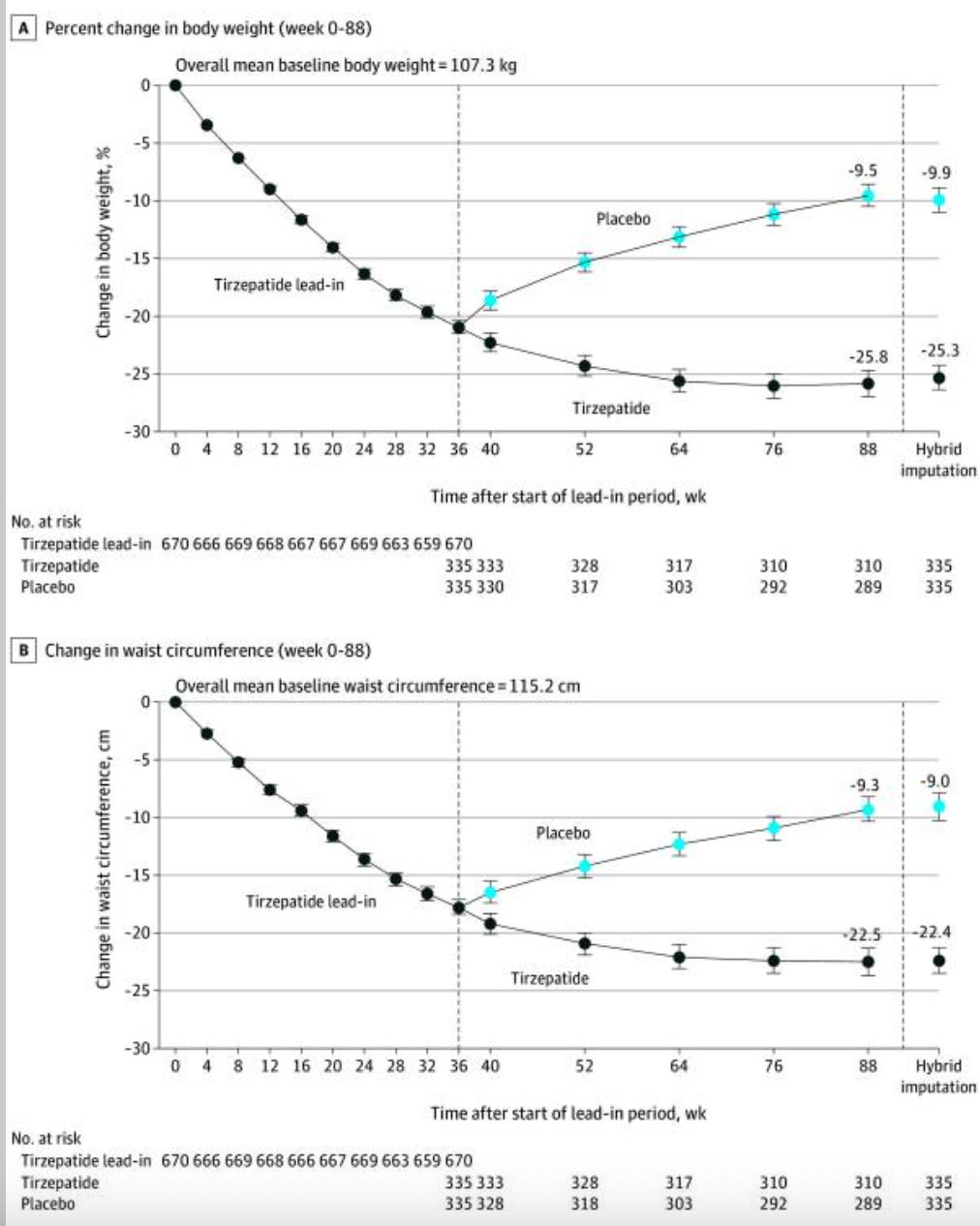
uh oh….
STEP 1’s off-treatment extension is even more sobering. After losing 17.3% on semaglutide over 68 weeks, participants discontinued everything; medication and lifestyle program. Within one year, they regained two-thirds of their lost weight!
A 2025 meta-analysis synthesising multiple discontinuation studies found that after one year off GLP-1s, people regain approximately 60% of weight lost.
The trajectory follows a predictable pattern: rapid initial recovery, gradual tapering, eventual plateauing below the original baseline.
Long-term, perhaps 25% of initial weight loss persists; translating to 4-5% reduction from baseline.
Why? Because stopping the medication removes its effects on brain appetite centres. Hunger increases. Satiety decreases. Metabolic rate, which dropped during weight loss, remains suppressed.
Ghrelin rises. Leptin falls.
The body’s biological drive to restore lost weight kicks into high gear.
We (usually) don’t expect people with hypertension to stop their blood pressure medication once their readings normalise. We (usually) don’t tell diabetics to discontinue insulin after achieving target glucose levels.
Obesity is a chronic disease with chronic metabolic, hormonal, and neurological drivers. Treating it requires ongoing intervention.
The rebound data confirms what we’ve learned from decades of weight-loss research: sustainable treatment of obesity requires continuous therapy. Whether that’s lifelong medication, bariatric surgery’s anatomical changes, or some combination….the “cure and stop” model doesn’t work.
My thoughts as a gastroenterologist
In my opinion GLP-1 receptor agonists represent a genuine breakthrough.
The weight loss magnitude. The cardiovascular benefits. The metabolic improvements. The quality-of-life enhancements. These are real, substantial, evidence-based benefits.
The need NOT to potentially re-arrange your anatomy.
GLP-1 agonists work best within comprehensive care. They require proper medical oversight, not DIY approaches or online quick prescriptions.
My patients need ongoing monitoring; kidney function, gallbladder surveillance, body composition assessment, nutritional adequacy (muscle composition especially), mental health support.
Sixty-seven percent of primary care physicians expressed concern about third-party telehealth GLP-1 access risking patient health.
I share that concern.
The rise of direct-to-consumer platforms that reduce complex medical care to a transaction….that bypass comprehensive evaluation, proper titration, adequate follow-up….troubles me deeply.
These medications can delay gastric emptying. That matters for surgery and procedures. They can cause dehydration with GI symptoms. They require dose escalation protocols to minimise side effects. They interact with other medications. They’re contraindicated in certain populations. None of this lends itself to a checkbox questionnaire and overnight prescription.
The FDA has reported 392 adverse events with compounded semaglutide and 215 with compounded tirzepatide, including multiple hospitalisations from dosing errors.
The black market flood of counterfeit products, incorrectly dosed medications, and contaminated compounds poses genuine danger.
Here’s what I tell patients considering GLP-1 therapy:
This is a commitment. A chronic treatment for a chronic disease. You’ll likely need lifelong medication; or you’ll regain weight. You need comprehensive lifestyle modification: resistance training to preserve muscle, adequate protein intake, nutritional counselling, behavioural support. You need proper medical supervision: baseline labs, regular monitoring, specialist involvement when indicated, multidisciplinary care coordination.
Here is my guide to working out here
And you need realistic expectations. These medications produce substantial weight loss. But they don’t solve everything. They won’t address the underlying psychological relationships with food. They won’t fix the food environment. They won’t eliminate all health risks.
They are, however, the most effective obesity pharmacotherapy we’ve ever had. For many people, those who haven’t responded to lifestyle interventions, those with weight-related co-morbidities, those facing metabolic complications, they represent a genuinely transformative option.
Used appropriately. With proper oversight. As part of comprehensive care.
That’s the key qualifier: used appropriately.
And the future….
…looks promising.
Triple agonists targeting GLP-1, GIP, and glucagon receptors are showing preclinical results that normalise body weight in animal models; something never achieved before with pharmacotherapy alone.
Retatrutide demonstrated 24% weight loss at 48 weeks in Phase 2 trials.
Oral formulations are advancing. Novel combinations are emerging.
Personalised approaches based on individual metabolic profiles, co-morbidities, and treatment goals are on the horizon.
But the fundamental principles won’t change. Obesity is a chronic disease. Effective treatment requires chronic intervention.
Biology will defend against weight loss.
And comprehensive medical care (and NOT isolated medication dispensing) remains essential.
I’m cautiously optimistic. These medications have changed the landscape. They’ve given us powerful tools to address a disease that affects 40% of adults and contributes to tremendous suffering.
GLP-1s work.
The question is whether we’ll use them wisely. With appropriate oversight, comprehensive support, realistic expectations, and recognition that they’re one component of multimodal care rather than standalone solutions.
Struggling with liver or digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References
- Emmerich SD, Fryar CD, Stierman B, Ogden CL. Obesity and Severe Obesity Prevalence in Adults: United States, August 2021–August 2023. NCHS Data Brief, No. 508. National Center for Health Statistics. 2024. doi: 10.15620/cdc/159281
- NCD Risk Factor Collaboration. Worldwide trends in underweight and obesity from 1990 to 2022. Lancet. 2024;403:2162-2203. doi: 10.1016/S0140-6736(23)02750-2
- Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 Suppl):222S-225S. doi: 10.1093/ajcn/82.1.222S
- Zenténius E, et al. Self-Reported Weight-Loss Methods and Weight Change: Ten-Year Analysis in the Swedish Obese Subjects Study Control Group. Obesity. 2018;26(6):1023-1030. doi: 10.1002/oby.22200
- Sjöström L, et al. Review of the key results from the Swedish Obese Subjects (SOS) trial. Journal of Internal Medicine. 2013;273(3):219-34. doi: 10.1111/joim.12012
- Sjöström L, et al. Effects of Bariatric Surgery on Mortality in Swedish Obese Subjects. N Engl J Med. 2007;357:741-752. doi: 10.1056/NEJMoa066254
- Schauer PR, et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes — 5-Year Outcomes. N Engl J Med. 2017;376(7):641–651. doi: 10.1056/NEJMoa1600869
- Drucker DJ. Mechanisms of Action and Therapeutic Application of Glucagon-like Peptide-1. Cell Metab. 2018;27:740-756. doi: 10.1016/j.cmet.2018.03.001
- Wilding JPH, Batterham RL, Calanna S, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384:989-1002. doi: 10.1056/NEJMoa2032183
- Garvey WT, Batterham RL, Bhatta M, et al. Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial. Nat Med. 2022;28:2083-2091. doi: 10.1038/s41591-022-02026-4
- Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022;387:205-216. doi: 10.1056/NEJMoa2206038
- Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med. 2016;375:1834-1844. doi: 10.1056/NEJMoa1607141
- Rubino D, Abrahamsson N, Davies M, et al. Effect of continued weekly subcutaneous semaglutide vs placebo on weight loss maintenance in adults with overweight or obesity: the STEP 4 randomized clinical trial. JAMA. 2021;325:1414-1425. doi: 10.1001/jama.2021.3224
- Wilding et al. Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022;24(8):1553-1564.
- Aronne LJ, Sattar N, Horn DB, et al. Continued Treatment With Tirzepatide for Maintenance of Weight Reduction in Adults With Obesity: The SURMOUNT-4 Randomized Clinical Trial. JAMA. 2024;331:38-48. doi: 10.1001/jama.2023.24945
- Sodhi M, et al. Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss. JAMA. 2023;330(18):1795-1797.
- Postlethwaite TL, et al. Acute Pancreatitis Incidence in Patients Initiating Glucagon-Like Peptide-1 Receptor Agonists for Obesity in a Large US Health Care System. Diabetes Care. 2024;47(11):1981-1988.
- Pasternak B, et al. Use of glucagon-like peptide 1 receptor agonists and risk of serious renal events: Scandinavian cohort study. BMJ. 2024;384:e078242.
- Bezin J, et al. GLP-1 Receptor Agonists and the Risk of Thyroid Cancer. Diabetes Care. 2023;46(2):384-390.
- American Diabetes Association. Standards of Care in Diabetes—2025. Diabetes Care. 2025;48(Supplement_1):S1-S322. doi: 10.2337/dc25-SINT
- NICE. Semaglutide for managing overweight and obesity [TA875]. 2025.
- Mozaffarian D, Agarwal M, Aggarwal M, et al. Nutritional priorities to support GLP-1 therapy for obesity. Obesity. 2025;33:e24336. doi: 10.1002/oby.24336
- Shada A, Stem M, Funk LM, et al. Multisociety Clinical Practice Guidance for Safe Use of GLP-1 Receptor Agonists in Perioperative Period. Clin Gastroenterol Hepatol. 2024. doi: 10.1016/S1542-3565(24)00910-8
- FDA. Concerns with Unapproved GLP-1 Drugs Used for Weight Loss. 2024.
- Knerr PJ, Mowery SA, Finan B, et al. Next generation GLP-1/GIP/glucagon triple agonists normalize body weight in obese mice. Mol Metab. 2022;63:101533. doi: 10.1016/j.molmet.2022.101533
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamshire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.

