Bile acid malabsorption affects 30% of patients with unexplained diarrhoea
Chronic diarrhoea….that just won’t go away.
Despite a normal coeliac and thyroid screen, stool tests and colonoscopy the symptoms were persistent.
Upon direct questioning, the diarrhoea started shortly after the gallbladder was removed.
After getting a SeHCAT scan (will explain later) to confirm the diagnosis, the symptoms vanished after starting appropriate treatment.
Bile Acid Malabsorption (BAM) is an under diagnosed condition with strong medical evidence for effective treatments. Sadly, the average patient suffers for years before receiving proper diagnosis and care.
Recent randomised controlled trials demonstrate that 60-96% of patients achieve symptom relief with proper treatment, yet awareness remains surprisingly low among both patients and healthcare providers.
What is bile acid malabsorption (BAM)?
Bile acids are powerful detergent-like molecules your liver produces to digest fats.
Under normal circumstances, your body operates a smart recycling system called the enterohepatic circulation.
Your liver produces about 3-5 grams of bile acids daily, but your intestines reabsorb 95% of them, cycling this resource 4-6 times per day.
This recycling happens primarily in the terminal ileum, the last section of your small intestine, through specialised transport proteins The most important is the apical sodium-dependent bile acid transporter (ASBT), which captures bile acids and shuttles them back to your liver via the bloodstream.
In bile acid malabsorption, this recycling system breaks down.
Instead of being reabsorbed, excess bile acids escape into your colon where they don’t belong. These wayward bile acids act like intestinal irritants, triggering water secretion, increased motility, and inflammation….the perfect storm for chronic diarrhoea
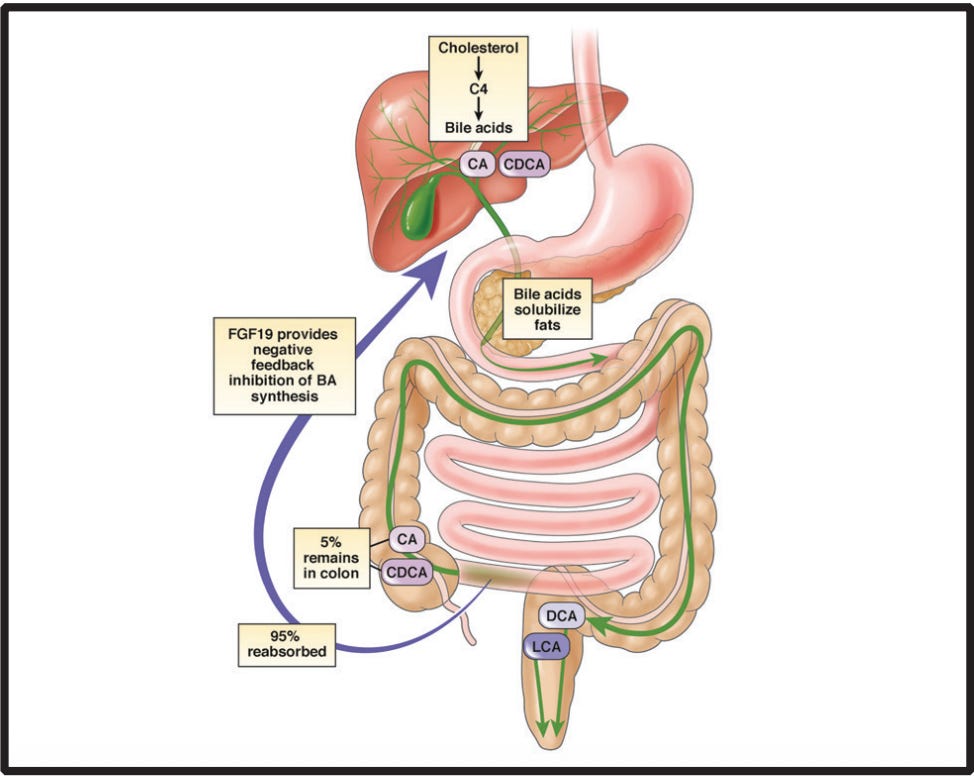
Enterohepatic circulation of bile acids. BA, bile acid; CA, cholic acid; CDCA, chenodeoxycholic acid; DCA, deoxycholic acid; LCA, lithocholic acid; FGF, fibroblast growth fact 19; C4, 7-α-hydroxy-4- cholesten-3-one.
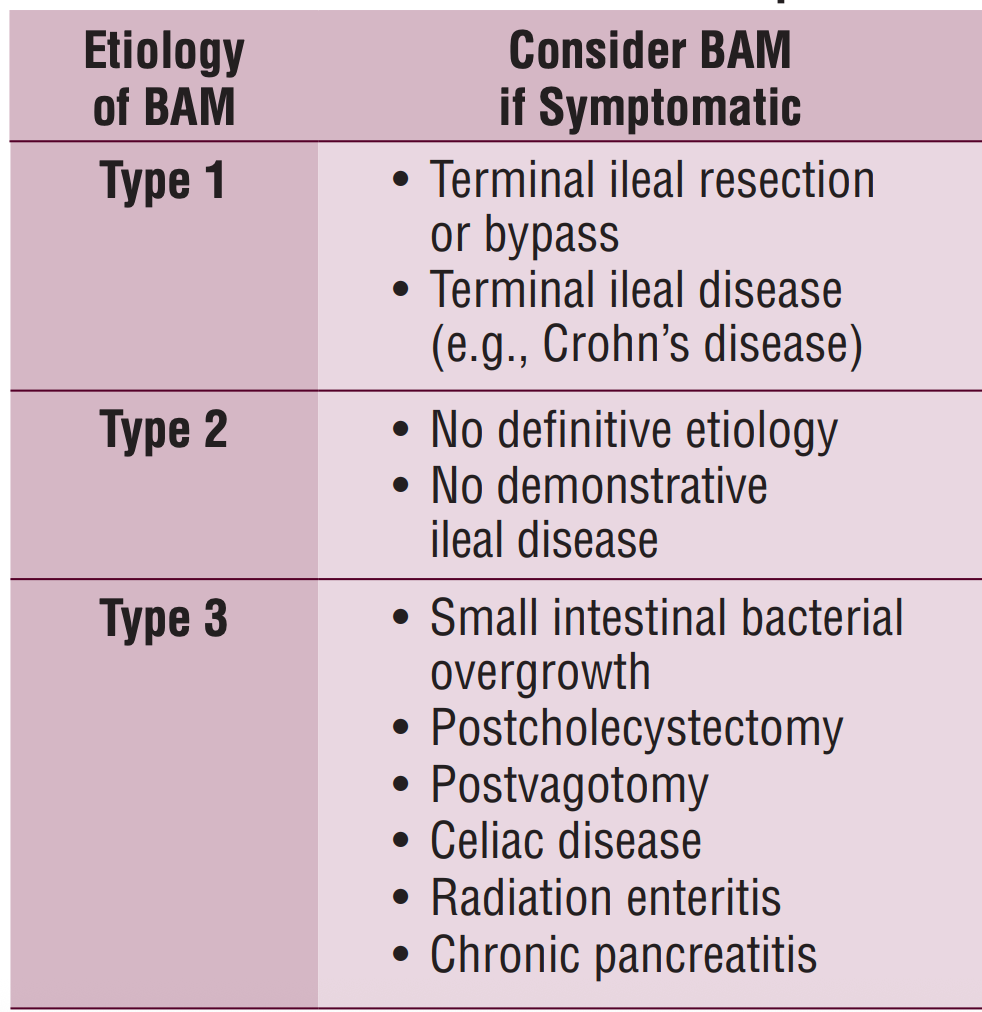
The condition manifests in several forms.
- When the terminal ileum is damaged by diseases like Crohn’s or surgical removal.
- Gallbladder removal (this organ stores bile)
- Idiopathic (no specific cause identified)
- Deficiency in FGF19, a hormone that normally tells your liver to stop making bile acids. Without adequate FGF19 signalling, your liver keeps producing bile acids without an off switch, overwhelming your intestine’s reabsorption capacity.
https://med.virginia.edu/ginutrition/wp-content/uploads/sites/199/2020/05/Bile-Acid-Malabsorption-May-2020.pdf
The 30% statistic….
The landmark finding that transformed our understanding of chronic diarrhoea came from a 2009 systematic review. Analysing 18 studies comprising 1,223 patients with IBS-D, researchers found that 32% had moderate bile acid malabsorption when tested with the gold-standard SeHCAT scan.
A 2015 updated meta-analysis confirmed that “in excess of one quarter of patients meeting accepted criteria for IBS-D have bile acid malabsorption.
A 2021 prospective study found 52.6% of patients with chronic functional diarrhoea tested positive when stringent diagnostic criteria were applied.
Bile acid malabsorption affects approximately 1% of the general adult population, making it more common than inflammatory bowel disease (Ulcerative Colitis and Crohn’s disease)
Who develops bile acid malabsorption
Post-cholecystectomy patients face the highest documented risk. A systematic review found that gallbladder removal increases BAM risk by 2.5-fold.
The mechanism involves continuous bile flow into the intestine without the gallbladder’s storage function. This steady stream can overwhelm the terminal ileum’s reabsorption capacity, particularly in patients who already have subtle absorption defects.
Terminal ileum disorders represent another major risk category. Crohn’s disease with ileal involvement carries a 12.4-fold increased risk, with high prevalence in patients with ileal resection (a potential surgical treatment for Crohn’s disease).
Less recognised but increasingly important is metformin-induced BAM.
Multiple randomised controlled studies demonstrate that this common diabetes medication reduces ileal bile acid reabsorption. In one double-blind crossover trial, metformin significantly increased faecal bile salt excretion and stool liquidity compared to placebo. This type of BAM can develop after years of metformin use and is often misdiagnosed as IBS.
Other evidence-based risk factors include radiation therapy (especially radiation to the abdomino-pelvic region), microscopic colitis, coeliac disease, and chronic pancreatitis.
Recognising the telltale symptoms
The hallmark symptom is watery, non-bloody diarrhoea
The stool may also be discoloured (green, yellow, orange) due to excess bile pigments.
Urgency, faecal incontinence and unpredictability are also features of BAM.
Fat-rich meals consistently trigger symptoms because dietary fat stimulates bile acid release.
Anxiety around social gatherings ?where is the nearest bathroom is common.
Less understood symptoms include abdominal cramping, excessive flatulence, bloating, and even “brain fog”. The neurological symptoms likely reflect the inflammatory cascade triggered by chronic bile acid exposure in the gut.
The treatment response pattern provides another diagnostic clue. Systematic reviews show dose-dependent response rates: 96% in severe BAM, 80% in moderate BAM, and 70% in mild BAM when treated with bile acid sequestrants.
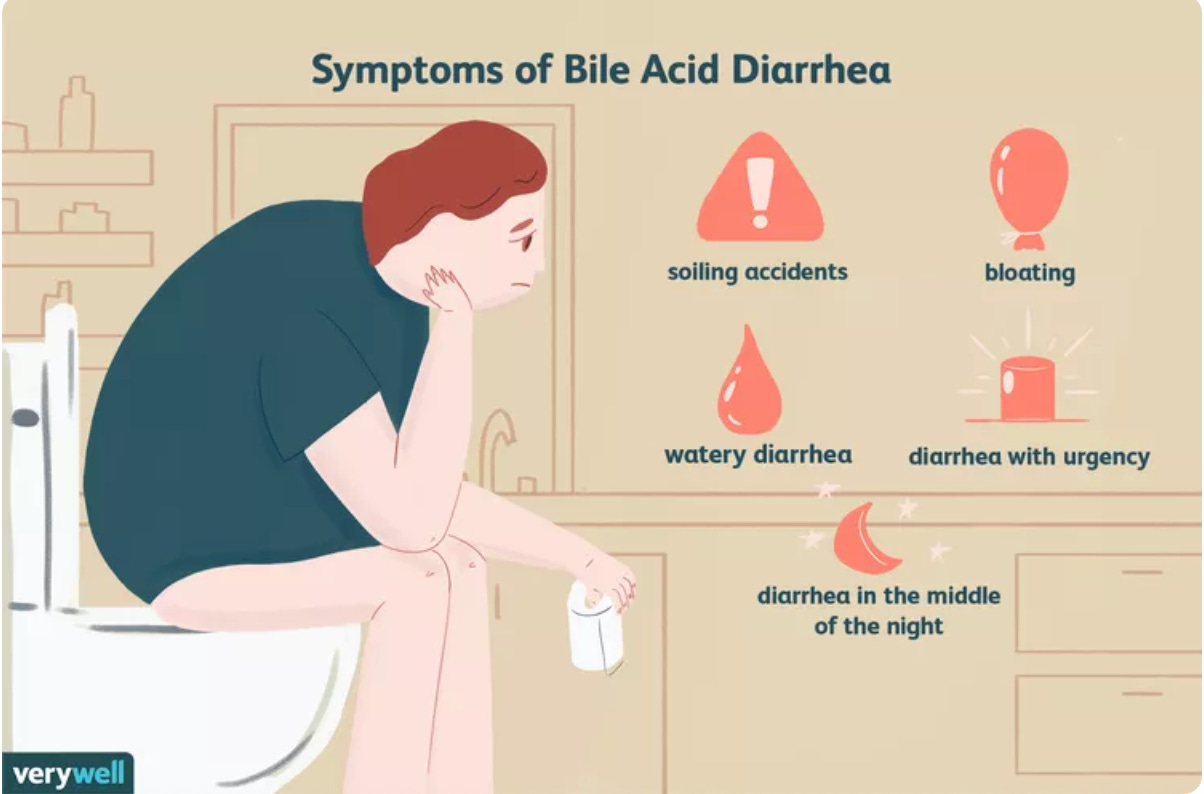
https://www.verywellhealth.com/bile-acid-diarrhea-1945221 – Credit: Nusha Ashjaee
Red flags that point elsewhere
Blood in watery stool represents a red flag because BAM causes secretory diarrhoea without mucosal damage. Any rectal bleeding, melaena, or positive qFIT (microscopic blood in stool) test requires investigation for other causes like inflammatory bowel disease or colorectal cancer.
Significant unexplained weight loss exceeding 5kg over three months should trigger alarm bells. Functional disorders like BAM typically don’t cause substantial weight loss unless accompanied by depression or anxiety severe enough to affect eating.
Persistent fever accompanying diarrhoea suggests infectious or inflammatory or infective processes incompatible with BAM.
New-onset chronic diarrhoea after age 50 requires cancer screening regardless of other symptoms. UK guidelines recommend urgent evaluation within two weeks for this population.
Strong family history of inflammatory bowel disease, colon cancer, or coeliac disease should prompt specific screening tests even if BAM is suspected. These conditions can coexist or predispose to secondary BAM.
Laboratory red flags include elevated inflammatory markers (CRP) suggesting IBD, severe anaemia beyond what chronic disease typically causes, or significant electrolyte abnormalities indicating secretory pathogens.
The gold standard diagnosis
The SeHCAT scan remains the definitive diagnostic test where available.
This nuclear medicine procedure uses a radioactive bile acid analog that mimics natural bile acid behaviour in your body.
You swallow a small capsule containing the tracer, then return exactly seven days later for a second scan. The gamma camera measures how much tracer remains in your body.
Normal retention exceeds 15%, while values below 15% indicate progressive degrees of malabsorption.
Diagnostic accuracy is impressive: 87.32% sensitivity and 93.2% specificity according to systematic review data.
The test carries minimal radiation exposure equivalent to two months of natural background radiation.
Alternative tests exist but are rarely used in clinical practice. Serum C4 and FGF19 blood tests offer reasonable sensitivity but limited specificity, while 48-hour faecal bile acid measurement remains cumbersome and impractical for routine use.
Where testing is unavailable, therapeutic trials with bile acid sequestrants remain a valid approach.
Evidence-based treatment approaches
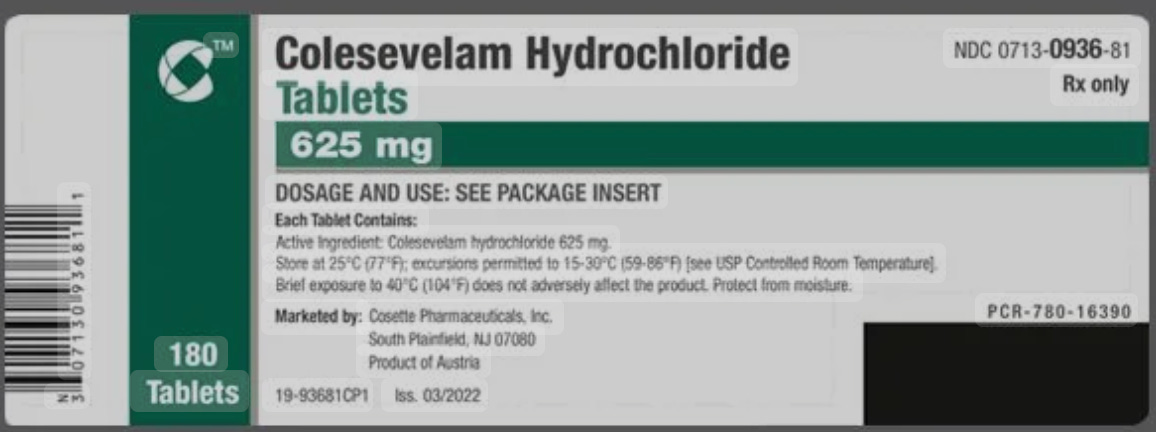
Bile acid sequestrants represent first-line therapy with strong RCT evidence.
These medications work by binding bile acids in your intestine, preventing their irritating effects on the colon while allowing natural replacement through normal synthesis.
Colesevelam emerges as the preferred option based on superior tolerability and convenience. The SINBAD trial, a phase 4 randomised controlled study of 168 patients, demonstrated 64% remission rates in C4-defined BAM patients versus 16% with placebo. Another double-blind RCT in Crohn’s disease showed 69.7% of patients achieved meaningful symptom reduction compared to 27.3% with placebo.
Standard colesevelam dosing starts at 1.25 grams twice daily, titrated based on response up to 3.75 grams daily. In my opinion the tablet form offers significant advantages over powder formulations—better taste tolerance, improved compliance, and easier administration.
Cholestyramine remains widely available and effective despite tolerability challenges. Response rates range from 70-96% across multiple studies, with systematic reviews showing 96% response in severe BAM. Starting doses of 4 grams once or twice daily can be increased to 16 grams daily.
Timing and drug interactions require careful attention. Other medications should be taken 1 hour before or 4-6 hours after bile acid sequestrants to prevent absorption interference. Critical interactions include warfarin, thyroid hormones, and fat-soluble vitamins. Taking sequestrants with meals improves tolerance without affecting efficacy.
Response typically occurs within 1-2 weeks, with full assessment requiring 4-6 weeks. Long-term studies show 67% of patients continue treatment at four-year follow-up, with some achieving sustained remission after discontinuation.
Common side effects include constipation and flatulence, though colesevelam causes significantly fewer gastrointestinal complaints than first-generation sequestrants. Serious contraindications include complete biliary obstruction, bowel obstruction, and raised triglyceride levels.
Dietary strategies??
Evidence-based dietary modification centres on fat restriction to 20% of total daily energy intake. A small prospective study of 40 patients with confirmed BAM showed statistically significant improvement in urgency, bloating, and bowel frequency when fat intake was reduced by approximately 42 grams daily
The mechanism is straightforward; reducing dietary fat decreases bile acid secretion demand, minimising the excess bile acids that trigger colonic symptoms. This creates a more manageable load for compromised absorption systems.
Small, frequent meals work better than large meals because they provide steadier bile acid stimulation rather than overwhelming surges. Strategic meal timing can help patients manage their symptom patterns throughout the day.
Soluble fibre supplementation may show promise based on mechanistic studies demonstrating bile acid binding properties. Sources like oats, bananas, chia seeds, and psyllium create viscous matrices that may trap bile acids (more evidence needed).
Practical implementation requires professional guidance. Working with a registered dietitian helps ensure nutritional adequacy while achieving symptom control.
Fat-soluble vitamin monitoring becomes essential with sustained low-fat diets, as both BAM itself and dietary restriction can impair absorption of vitamins A, D, E, and K.
Sample modifications include replacing butter with low-fat alternatives, choosing lean protein sources, using fat-free cooking methods, and reading labels for hidden fats. Many patients find that avoiding large, fat-heavy meals provides immediate symptom relief while awaiting medication effects.
However, strong dietary evidence for BAM is limited. High-quality randomised controlled trials specifically testing dietary interventions in BAM patients are urgently needed to strengthen recommendations
The path forward
Bile acid malabsorption represents a common cause of chronic diarrhoea. With 30% of unexplained diarrhoea cases having BAM, physicians must move beyond defaulting to IBS diagnoses and systematically evaluate for this treatable condition.
The barriers are clear: limited SeHCAT availability outside Europe, (possibly) inadequate provider awareness (however, certainly improving with non-gastroenterologists), and the misconception that BAM is rare.
For patients with risk factors: cholecystectomy, ileal disease, or metformin use, advocacy for testing can be life-changing. The combination of dietary modification and bile acid sequestrants offers genuine hope for symptom control.
The evidence is clear: bile acid malabsorption is common, diagnosable, and treatable. The question isn’t whether it affects your patients…it’s whether you’re looking for it.
Struggling with digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References
- Slattery SA, Niaz O, Aziz Q, Ford AC, Farmer AD. Systematic review with meta-analysis: the prevalence of bile acid malabsorption in the irritable bowel syndrome with diarrhoea. Aliment Pharmacol Ther. 2015;42(1):3-11.
- Fernández-Bañares F, Rosinach M, Piqueras M, et al. Prevalence of biliary acid malabsorption in patients with chronic diarrhoea of functional characteristics: a prospective study. BMC Gastroenterol. 2021;21(1):66.
- Wedlake L, A’Hern R, Russell D, Thomas K, Walters JR, Andreyev HJ. Systematic review: the prevalence of idiopathic bile acid malabsorption as diagnosed by SeHCAT scanning in patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2009;30(7):707-17.
- Borup C, Vinter-Jensen L, Jørgensen SP, et al. A positive SeHCAT test results in fewer subsequent investigations in patients with chronic diarrhoea. Frontline Gastroenterol. 2017;8(4):279-283.
- Vijayvargiya P, Camilleri M, Chedid V, Carlson P, Busciglio I, Burton D. Methods for diagnosing bile acid malabsorption: a systematic review. BMC Gastroenterol. 2019;19(1):185.
- Bajor A, Törnblom H, Rudling M, Ung KA, Simrén M. Increased colonic bile acid exposure: a relevant risk factor for symptoms and treatment in IBS. Gut. 2015;64(1):84-92.
- Wilcox C, Turner J, Green J. Systematic review: the management of chronic diarrhoea due to bile acid malabsorption. Aliment Pharmacol Ther. 2014;39(9):923-39.
- Vijayvargiya P, Camilleri M. Current practice in the diagnosis of bile acid diarrhea. Gastroenterology. 2019;156(5):1233-1238.
- Camilleri M, Acosta A, Busciglio I, et al. Effect of colesevelam on faecal bile acids and bowel functions in diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2015;41(5):438-48.
- Walters JR, Johnston IM, Nolan JD, Vassie C, Pruzanski ME, Shapiro DA. The response of patients with bile acid diarrhoea to the farnesoid X receptor agonist obeticholic acid. Aliment Pharmacol Ther. 2015;41(1):54-64.
- Barkun AN, Love J, Gould M, Pluta H, Steinhart AH. Bile acid malabsorption in chronic diarrhea: pathophysiology and treatment. Can J Gastroenterol. 2013;27(11):653-9.
- Pattni S, Walters JR. Recent advances in the understanding of bile acid malabsorption. Br Med Bull. 2009;92:79-93.
- Watson L, Lalji A, Bodla S, Muls A, Andreyev HJ, Shaw C. Management of bile acid malabsorption using low-fat dietary interventions: a useful strategy applicable to some patients with diarrhoea-predominant irritable bowel syndrome? Clin Med (Lond). 2015;15(6):536-40.
- Mottacki N, Simrén M, Bajor A. Review article: bile acid diarrhoea – pathogenesis, diagnosis and management. Aliment Pharmacol Ther. 2016;43(8):884-98.
- Valentin N, Camilleri M, Carlson P, et al. Potential mechanisms of effects of serum-derived bovine immunoglobulin/protein isolate therapy in patients with diarrhea-predominant irritable bowel syndrome. Physiol Rep. 2017;5(5):e13170.
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.

