Colorectal cancer is rising amongst younger adults; here are some tips to lower your risk
“I’m sorry…there are no curative options.”
These devastating words hung in the air as I faced the young woman across from me during an urgent “breaking bad news” clinic.
At just forty-something, with three children and no previous health concerns, she had received an unimaginable diagnosis…
Advanced bowel cancer that had already spread extensively to her liver and lungs.
Her symptoms began six months earlier with subtle warning signs…rectal bleeding mixed with stools, followed by increasingly loose bowel movements.
Only when fatigue and unexplained weight loss set in did she seek medical attention.
The subsequent colonoscopy and CT scan confirmed our worst fears.
I share this heartbreaking story not to dampen your day, but as a stark reminder: recognising early warning signs, understanding risk factors, and taking preventative action could save your life when it comes to colorectal cancer.
What are the stats?
Colorectal cancer (CRC) is the third most common cancer around the world.
The European Union experienced over 1.2 million cancer deaths in 2024, with CRC mortality rates declining by 4.8% for men and 9.5% for women since 2018.
A concerning trend emerges when examining the global burden of CRC over time. Between 1990 and 2021, incident cases, deaths, and disability-adjusted life years (DALYs) attributed to CRC have doubled worldwide.
While age-standardised death rates exhibit a decreasing trend overall, the age-standardised incidence rate (ASIR) has shown a slight upward tendency.
Younger people with colorectal cancer?
Perhaps most concerning is the notable shift toward younger onset of colorectal cancer. Incidence rates have increased by 1%-2% annually for colorectal cancers in adults younger than 55 years. This trend has dramatically altered the landscape of cancer mortality among young adults; colorectal cancer was the fourth-leading cause of cancer death in individuals younger than 50 years in the late 1990s but is now the first cause in men and the second in women within this age group.
The percentage of cases among individuals younger than 55 years has increased from 11% in 1995 to 20% in 2019. This may be due to better screening or because of possible risk factors.
Why are we seeing this trend?
Scientists are still discovering why colorectal cancer is becoming more common in people under 50, and the answer lies in everyday lifestyle choices. Three main factors stand out: obesity, diet, and our gut microbiome.
Being overweight, especially during teenage years or early adulthood, nearly doubles the risk of developing colorectal cancer. This happens because excess body fat triggers long-lasting inflammation and insulin resistance. Childhood obesity may be associated with an increased risk of developing cancer.
Diet plays a crucial role too. The typical Western diet, packed with processed meats with low fibre, damages DNA directly and throws off the balance of gut bacteria. A study identified specific strains of E. coli that produce a toxin called colibactin, which damages DNA and is particularly common in younger cancer patients.
Together, these factors create an inflammatory environment in the colon may lead to cancer development…even in people without genetic predisposition. The key insight? What happens early in life, from childhood through young adulthood, may set the stage for cancer decades later.
(Almost) all cancer starts of as a polyp, however not all polyps turn into cancer….most remain benign.
So what not to do?
Be embarrassed / not talk about your symptoms
I get it…talking about your “number two” can be embarrassing but trust me when I say this….
There is nothing you can say about your bowels that will shock or surprise your gastroenterologist or colorectal surgeon.
Firstly, don’t ignore blood in your stool. This is a common finding; you may find blood mixed in with your stool, in the pan or on wiping. Although this symptom can be attributed to an easily treated condition such as a fissure (small cut at the anal verge) or pile (haemorrhoid), it could also be a sign of something serious.
Next, give us the details. A change in bowel habit, night time symptoms, urgency, the feeling of incomplete emptying (tenesmus) or incontinence gives us clues to what could be going on.
If your symptoms are borderline, your specialist will likely request non-invasive tests including blood and stool samples to investigate further. A colonoscopy +/- CT scan would only be considered for red flag symptoms or if your non-invasive tests flagged something important.
Either way, it is far better to talk early about your symptoms and be reassured than save yourself from self perceived embarrassment and pay the price later down the line.
Ignore a family history
Family history plays a major role in colorectal cancer risk.
Over 25% of people who develop colorectal cancer at a young age have relatives who have had the disease.
Because of this strong connection, I recommend that all patients diagnosed with early-onset colorectal cancer speak to their specialist to review whether they are eligible to receive genetic counselling and testing for cancer-related genes.
Examples of inherited genetic conditions linked to bowel cancer are:
- Lynch Syndrome: The most common inherited form of colorectal cancer, caused by mutations in DNA repair genes (MLH1, MSH2, MSH6, PMS2, or EPCAM) that requires colonoscopy screening starting at age 20-25.
- Familial Adenomatous Polyposis (FAP): A rare inherited condition caused by APC gene mutations where almost all affected individuals will develop colorectal cancer without preventive intervention.
- MUTYH-Associated Polyposis (MAP): A recessively inherited disorder that causes distinctive colon polyps and colorectal cancers, typically located in the right side of the colon.
- Peutz-Jeghers Syndrome: A rare inherited condition marked by distinctive skin pigmentation and special polyps that increases colorectal cancer risk by over 200 times compared to the general population.

Blue-grey pigmentation in the lips…classic of Peutz Jeghers Syndrome
Miss / delay screening or a colonoscopy
Early detection saves lives, and we now have solid evidence showing which screening tests work best for catching colorectal cancer before it’s too late.
The simplest screening option is the quantitative faecal immunochemical test (qFIT); a non-invasive test you can do at home that checks for hidden blood in stool. However, its effectiveness depends on how advanced the cancer is. qFIT catches about half of the earliest stage cancers (52%), but performs much better for more developed tumours, detecting up to 93% of stage 3 cancers. This means qFIT is good but not perfect; it might miss some very early cancers when they’re most treatable.
Colonoscopy remains the gold standard for screening. Large studies following thousands of people show that regular colonoscopy cuts the risk of developing colorectal cancer by more than half (52%) and reduces deaths from the disease by an impressive 62%. During a colonoscopy, doctors can spot and remove pre-cancerous polyps before they turn dangerous, which explains why it’s so effective at prevention, not just detection.
Both tests save lives, but they work differently. qFIT offers convenience and catches most advanced cancers, while colonoscopy provides the most comprehensive protection by finding and removing problems early. The best screening test is the one you’ll actually do regularly.
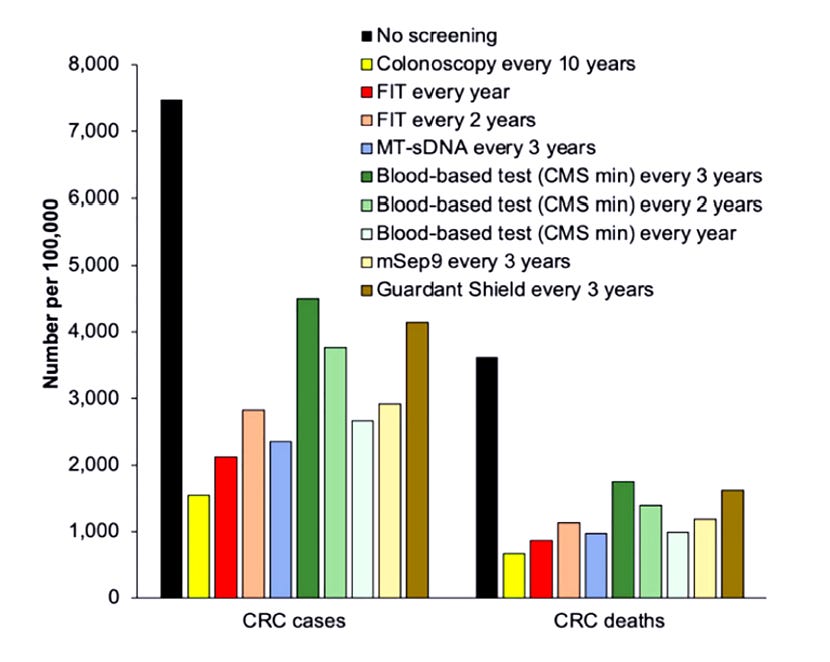
While colonoscopy is one of the most accurate screening tests available, offering it to everyone in the country is not practical due to the significant financial costs, staffing needs, and facility requirements. No screening test is perfect, but the resources needed for universal colonoscopy make it an unfeasible option.
Ignore lifestyle measures
Research involving thousands of people has revealed clear patterns about who is at higher risk for colorectal cancer and what we can do to lower that risk.
Highest Risk Factors: The strongest risk comes from inflammatory bowel disease (IBD), which nearly triples your chances of developing colorectal cancer. If you have Crohn’s disease or ulcerative colitis, regular screening discussions with your specialist are essential.
Having a parent, sibling, or child with colorectal cancer also matters significantly; it increases your risk.
Lifestyle Factors That Increase Risk:
- Weight: Every 8-point increase in BMI raises your risk by 10%
- Smoking: Even moderate smoking (5 pack-years) increases risk
- Red meat: Eating red meat 5 times per week raises risk by 13%
Protective Lifestyle Choices: The good news? You can actively lower your risk through simple daily choices:
- Exercise: Regular physical activity reduces risk by 12%
- Fruits: Eating 3 servings daily lowers risk by 15%
- Vegetables: Having 5 servings daily reduces risk by 14%
The rising rates of colorectal cancer in younger adults are alarming, but we are not powerless against this trend. While we can’t change our genetics, we can control many risk factors through daily choices.
Staying active, eating more fruits and vegetables, maintaining a healthy weight, and getting screened on time. Most importantly, don’t let embarrassment stop you from discussing symptoms or getting that colonoscopy; taking action today could save your life tomorrow.
Struggling with digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
Thanks for reading! The Gut Group helps you manage your liver and digestive issues through a regular newsletter: https://drhussenbux.substack.com/
References
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin. 2024 Jan-Feb;74(1):12-49. doi: 10.3322/caac.21820. Epub 2024 Jan 17. Erratum in: CA Cancer J Clin. 2024 Mar-Apr;74(2):203
- Zhou J et al. Evolving landscape of colorectal cancer: Global and regional burden, risk factor dynamics, and future scenarios (the Global Burden of Disease 1990-2050). Ageing Res Rev. 2025 Feb;104:102666
- Siegel RL et al. Colorectal cancer statistics, 2023. CA Cancer J Clin. 2023 May-Jun;73(3):233-254
- Zinkeng A et al. Early Onset Colorectal Cancer: Molecular Underpinnings Accelerating Occurrence. Cell Mol Gastroenterol Hepatol. 2025;19(2):101425.
- Johnson CM et al. Meta-analyses of colorectal cancer risk factors. Cancer Causes Control. 2013 Jun;24(6):1207-22
- Zhang J et al. Colonoscopic screening is associated with reduced Colorectal Cancer incidence and mortality: a systematic review and meta-analysis. J Cancer. 2020 Aug 15;11(20):5953-5970.
- Fitzpatrick-Lewis D et al. Screening for Colorectal Cancer: A Systematic Review and Meta-Analysis. Clin Colorectal Cancer. 2016 Dec;15(4):298-313
- Niedermaier T et al. Sensitivity of Faecal Immunochemical Test for Colorectal Cancer Detection Differs According to Stage and Location. Clin Gastroenterol Hepatol. 2020 Dec;18(13):2920-2928.
- Daca Alvarez M et al. The Inherited and Familial Component of Early-Onset Colorectal Cancer. Cells. 2021 Mar 23;10(3):710
- Vasen HF et al. Guidelines for the clinical management of familial adenomatous polyposis (FAP). Gut. 2008 May;57(5):704-13.
- Nielsen M et al. Colorectal carcinomas in MUTYH-associated polyposis display histopathological similarities to microsatellite unstable carcinomas. BMC Cancer. 2009 Jun 15;9:184.
- Chen HY et al. Cancer risk in patients with Peutz-Jeghers syndrome: A retrospective cohort study of 336 cases. Tumour Biol. 2017 Jun;39(6):1010428317705131.
- Adnan D et al. Early-onset Colon Cancer Shows a Distinct Intestinal Microbiome and a Host-Microbe Interaction. Cancer Prev Res (Phila). 2024 Jan 4;17(1):29-38
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.

