Most people who have gallstones never even knew they had them
Mr B underwent an abdominal ultrasound for vague symptoms.
The scan picked up multiple gallstones.
Quietly sitting in his gallbladder.
No classic gallbladder pain so he was reassured and discharged.
This left him with more questions.
“Should I be worried?”
“Do I need an operation?”
This scenario plays out daily in clinics worldwide.
Hopefully this article will answer these questions.
Most gallstones remain silent…discovered incidentally during imaging for other conditions.
Understanding when these stones transform from silent to medical concerns requires exploring their nature, formation, and the delicate balance between watchful waiting and intervention.
Join my newsletter….improving your liver and gut health…one e-mail at a time!
https://drhussenbux.substack.com/
Check out the video version here:
The Silent Majority
Gallstones affect approximately 10-15% of adults in Western populations, yet 80-85% remain asymptomatic throughout a person’s lifetime.
Among those with silent stones, only 1-4% develop symptoms annually, with the risk highest in the first five years after stone formation, then gradually declining.
A longitudinal study tracking asymptomatic gallstone patients found that 10% developed symptoms within five years, 20% within ten years, and 30% within fifteen years.
The remaining majority lived their entire lives without gallstone-related problems, their stones discovered only incidentally or at autopsy.
Stones of Different Colours
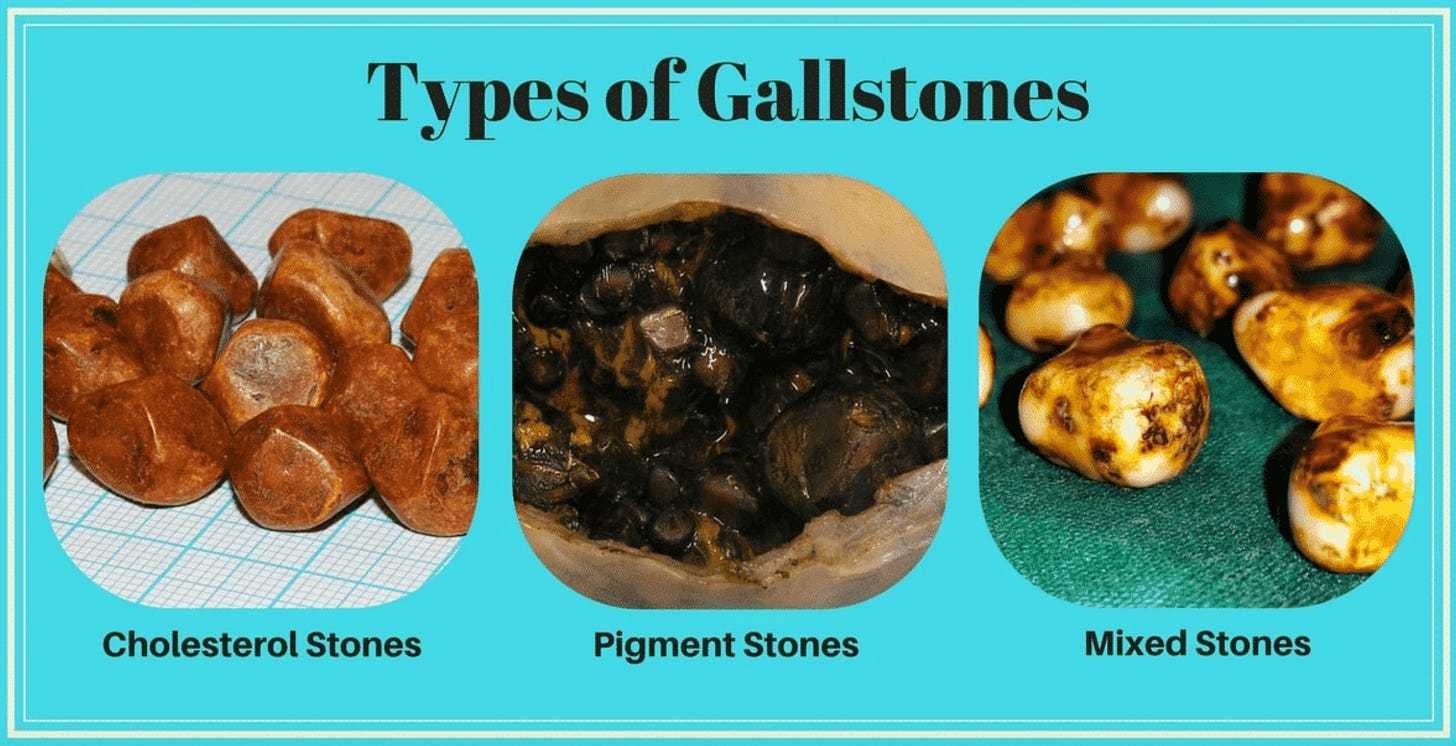
https://www.drvpareek.com/what-is-gall-stone-and-how-are-stones-formed-in-gallbladder/
In Western populations, cholesterol stones dominate, comprising 75-85% of cases.
These yellow-green stones form when bile becomes supersaturated with cholesterol, overwhelming the solubilising capacity of bile salts and phospholipids.
The forming stones can range from sand-grain sized to golf balls.
Black pigment stones, accounting for 15-20% of Western gallstones, form from calcium bilirubinate when unconjugated bilirubin precipitates in bile. They associate with haemolytic disorders, cirrhosis, and advancing age.
Brown pigment stones, rare in developed countries but common in Asia, result from bacterial action on bile components and often form within bile ducts rather than the gallbladder itself.
There is more to the “Four Fs”
The traditional mnemonic “female, forty, fat, and fertile” captures some gallstone risk factors but oversimplifies a complex picture.
Women face twice the gallstone risk of men, with oestrogen increasing cholesterol secretion into bile while progesterone reduces gallbladder emptying.
Pregnancy amplifies these effects, with each pregnancy increasing risk by approximately 2%.
Yet recent validation studies suggest updating this mnemonic. Age forty no longer stands as a clear threshold; risk increases gradually with age rather than spiking at forty.
First-degree relatives of gallstone patients face 2-4 times increased risk. Genetic factors account for approximately 25-30% of gallstone susceptibility.
Obesity remains a major modifiable risk factor, particularly central adiposity. Each 5-unit BMI increase raises gallstone risk by approximately 20%.
Paradoxically, rapid weight loss creates even higher risk than stable obesity. Weight loss exceeding 1.5 kg weekly can trigger gallstone formation in up to 25% of dieters, as the liver dumps excess cholesterol into bile while gallbladder motility decreases.
Modern Culprits: Weight Loss Medications and Surgery
The explosion of GLP-1 receptor agonists like Mounjaro (tirzepatide) and Ozempic (semaglutide) adds new complexity to gallstone epidemiology.
Meta-analysis of over 100,000 patients reveals these medications increase gallstone risk by approximately 37%, with higher doses and weight-loss indications carrying greater risk than diabetes treatment. The mechanism involves altered gallbladder motility and rapid weight loss effects on bile composition.
Bariatric surgery creates even more dramatic gallstone risk, with 30-50% of patients developing stones within two years post-surgery. The Swedish Obese Subjects Study documented significantly higher gallstone incidence in surgical patients over twenty years of follow-up.
The Mechanism of Gallstone related pain
https://www.narayanahealth.org/blog/biliary-colic-causes-symptoms-and-treatment-options
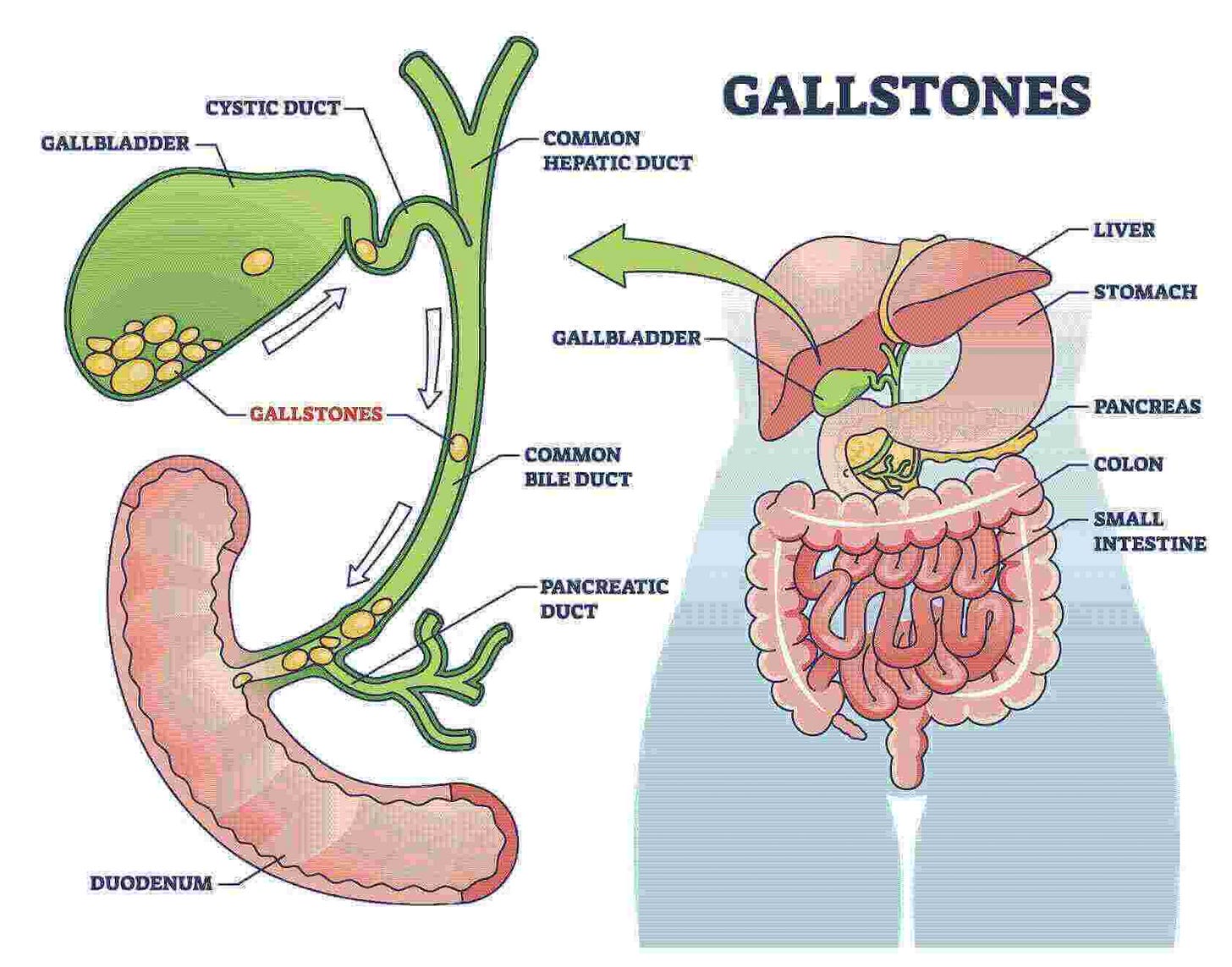
The gallbladder is a small sack that sits under the liver. It’s job is to store bile.
After eating, particularly fatty meals, the duodenum releases cholecystokinin (CCK), triggering gallbladder contraction, causing it to squeeze and release the bile.
The stone that was peacefully resting in the gallbladder lodges in the gallbladder neck or cystic duct….this creates pressure against the obstructing stone.
This pressure activates visceral pain fibres, creating “biliary colic” – a misnomer since the pain is steady, not colicky.
The classic presentation involves constant right upper quadrant pain lasting 30 minutes to several hours, often radiating to the back or right shoulder. The pain crescendos over 15-30 minutes, plateaus, then gradually resolves as the stone either passes or falls back into the gallbladder.
Complications arise when obstruction persists. Continued blockage leads to gallbladder inflammation (cholecystitis), requiring urgent intervention. If stones migrate into the common bile duct, they can cause jaundice, cholangitis, or pancreatitis…serious conditions requiring immediate attention.
A silent stone? Leave it alone!
Not much more to say here.
If the gallstone(s) sitting in your gallbladder are not causing any symptoms….no need for any intervention or follow up (in most cases!).
If there is a silent stone in your bile duct this needs a nuanced discussion with a gastroenterologist to weigh up the benefits and risks of intervening vs leaving alone.
When Inflammation Strikes
Acute cholecystitis represents the most common serious complication of gallstones, occurring when persistent cystic duct obstruction leads to gallbladder inflammation. The diagnosis relies on clinical findings – fever, right upper quadrant tenderness, combined with imaging showing gallbladder wall thickening and pericholecystic fluid.
Modern management strongly favours early laparoscopic cholecystectomy (gallbladder removal), ideally within 72 hours of symptom onset. The World Society of Emergency Surgery guidelines, based on multiple randomised trials, demonstrate that early surgery reduces total hospital stay by four days and allows return to work nine days sooner than delayed approaches.
The old practice of “cooling down” inflammation before surgery has been abandoned except in specific high-risk situations.
Stones in the bile duct

That’s an XR of a swollen bile duct absolutely packed with gallstones. Like a packet of smarties!
Common bile duct stones present unique challenges. These can form primarily in the ducts or migrate from the gallbladder. When stones obstruct bile flow, patients develop jaundice, dark urine, and pale stools. Add infection, and you have ascending cholangitis – a medical emergency requiring urgent intervention.
ERCP (Endoscopic Retrograde Cholangiopancreatography) is used for bile duct stone management. This procedure combines endoscopy with fluoroscopy to visualise and clear bile ducts. The procedure carries significant risk, making patient selection crucial. Read here for more! ERCP Guide
To conclude…
Most gallstones never announce themselves, living and dying as silent stones in asymptomatic gallbladders.
For those like Mr B with incidental findings, understanding the natural history of gallstones….their slow progression, predictable patterns, and clear warning signs transforms anxiety into informed watchfulness.
Join my newsletter….improving your liver and gut health…one e-mail at a time!
https://drhussenbux.substack.com/
Struggling with gallstones or digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References
- He L, Wang J, Ping F, et al. Association of Glucagon-Like Peptide-1 Receptor Agonist Use With Risk of Gallbladder and Biliary Diseases: A Systematic Review and Meta-analysis of Randomized Clinical Trials. JAMA Intern Med. 2022;182(5):513-519.
- Wan ZN, Tang Y, Li HY, et al. Global Epidemiology of Gallstones in the 21st Century: A Systematic Review and Meta-Analysis. Clin Gastroenterol Hepatol. 2024;22(8):1586-1595.
- Shabanzadeh DM, Sørensen LT, Jørgensen T. The Natural History of Asymptomatic Gallstones: A Longitudinal Study and Prediction Model. Clin Gastroenterol Hepatol. 2023;21(2):319-327.
- Pisano M, Allievi N, Gurusamy K, et al. 2020 World Society of Emergency Surgery updated guidelines for the diagnosis and treatment of acute calculus cholecystitis. World J Emerg Surg. 2020;15:61.
- Al-Musawi JHS, et al. Gastrointestinal safety of semaglutide and tirzepatide vs. placebo in obese individuals without diabetes: a systematic review and meta-analysis. Ann Saudi Med. 2024;44(2):129-142.
- Stenberg E, Dos Reis Falcão LF, O’Kane M, et al. Guidelines for Perioperative Care in Bariatric Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg. 2022;46(4):729-751.
- Wang HH, Portincasa P, Liu M, et al. Update on the Molecular Mechanisms Underlying the Effect of Cholecystokinin and Cholecystokinin-1 Receptor on the Formation of Cholesterol Gallstones. Curr Med Chem. 2021;28(18):3577-3598.
- de Mestral C, Kayssi A, Al-Omran M, et al. Validating the 5Fs mnemonic for cholelithiasis: time to include family history. Ann R Coll Surg Engl. 2013;95(6):436-440.

