“As soon as I stop it, the symptoms come back….”
Well that’s what my patient said to me the other day.
She had longterm acid reflux so went on to have a gastroscopy which was completely normal.
The endoscopist advised her to stop omeprazole, the acid suppression therapy medication (Proton Pump Inhibitor (PPI)) she had been taking regularly, everyday for over 5 years.
After a couple of months I saw her in Clinic:
“So Mrs P, how have you been? Have you managed to stay off omeprazole”.
And that was her reply to me…
Can you relate to her?
Are you one of the millions taking acid-reducing medications?
Do you know what happens in your body when you suppress stomach acid for months or years?
Have you ever wondered if that heartburn pill might be doing more than just relieving your symptoms?
Hopefully I can answer some of these questions today.
Acid-reducing medications, particularly proton pump inhibitors (PPI) like omeprazole, lansoprazole and esomeprazole are among the most commonly prescribed drugs worldwide.
Sadly, many patients I see in clinic don’t even know why they are on PPI.
While these medications provide critical relief for many, their long-term use deserves careful consideration.
Your Stomach Acid…More Important Than You Think
Your stomach’s acid production is a sophisticated system involving specialised cells and hormones working in perfect harmony.
In fact, you have been producing stomach acid your whole life!
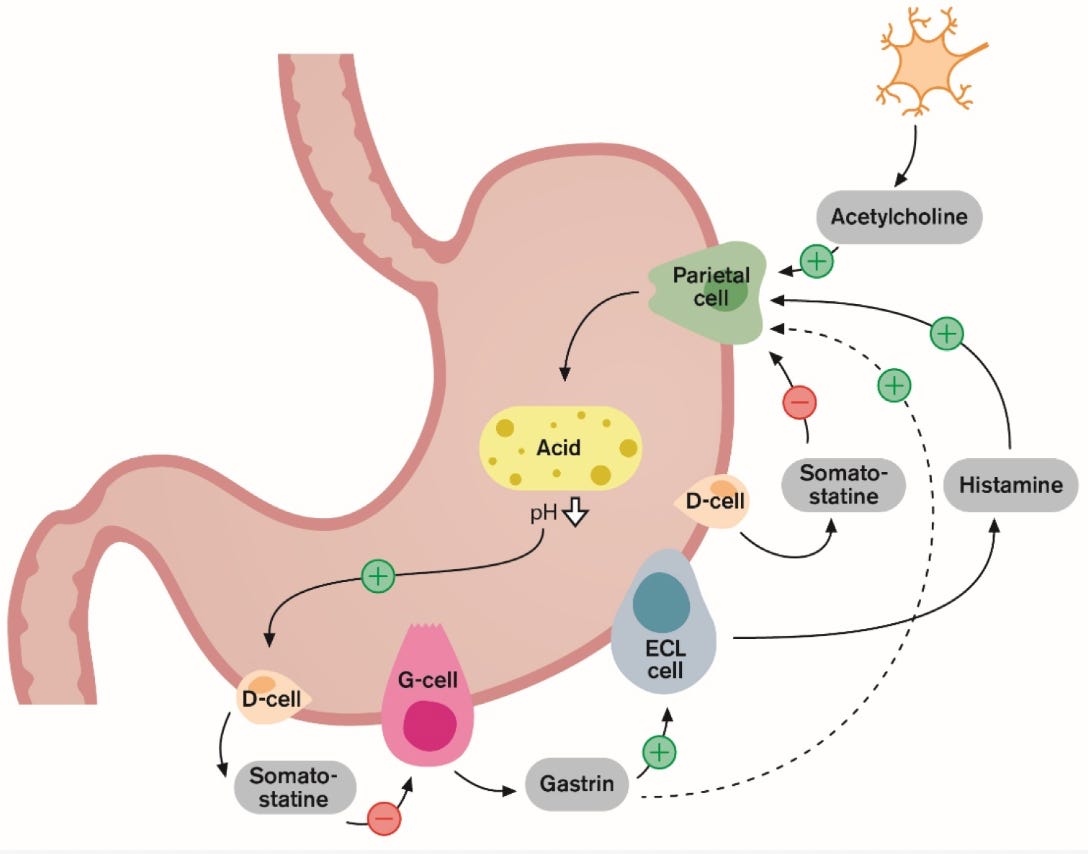
At the centre of this process are G cells, primarily located in the lower portion of your stomach.
G cells produce gastrin, a hormone that regulates acid production. When you eat protein, stretch your stomach with food, or even think about eating (triggering your vagus nerve), these G cells activate.
Once stimulated, G cells release gastrin into your bloodstream. This gastrin travels to acid-producing parietal cells, activating them through two pathways:
- Direct stimulation of parietal cells
- Triggering nearby enterochromaffin-like (ECL) cells to release histamine
Your parietal cells contain tiny biological pumps (the proton pumps) that actively push hydrogen ions into your stomach, creating hydrochloric acid.
This entire system is balanced by somatostatin-producing D cells, which create a feedback loop preventing excessive acid.
Simple, right? TLDR – you eat or even think about eating? Your body makes stomach acid.
You need to produce stomach acid
Yep – that’s the most important take home message of this whole article.
Your stomach acid isn’t just there to cause heartburn! It serves many crucial functions:
Stomach acid aids digestion: It creates the perfect environment for breaking down proteins and activates digestive enzymes
Nutrient Absorption: Essential for absorbing:
- Iron (preventing anaemia)
- Calcium (supporting bone health)
- Vitamin B12 (vital for nerve function)
- Many medications
Germ Defence: Your acidic stomach (typically pH 1-2) acts as a powerful antimicrobial barrier, killing many potential pathogens before they reach your intestines
Digestive Co-ordination: Triggers the release of pancreatic enzymes and bile, ensuring proper timing of the entire digestive process
There is a reason why PPIs are so commonly prescribed….
They work.
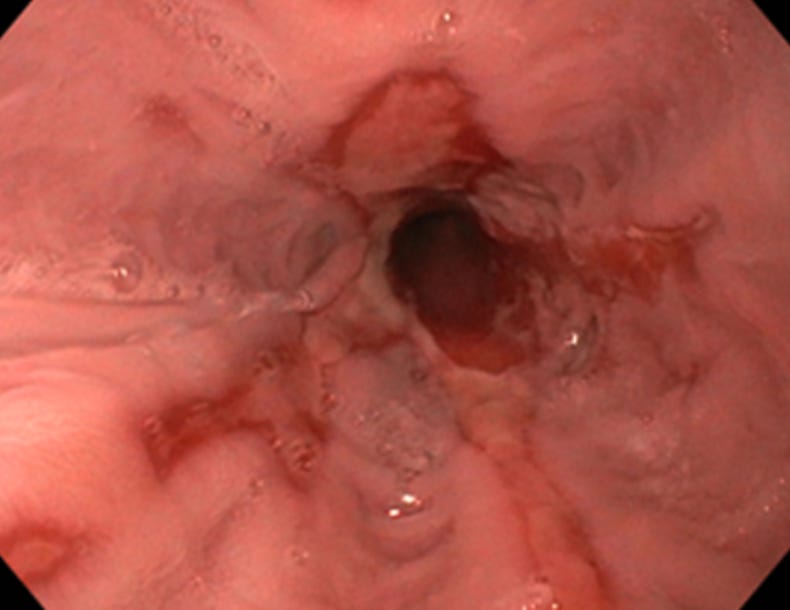
Oesophagitis…just a 6 week course of high dose PPI can get this oesophagus back to normal
When appropriately prescribed, PPIs offer important benefits:
- Powerful, consistent acid suppression without developing tolerance
- Effective treatment for conditions like GORD, ulcers, and H. pylori infections
- Protection against NSAID/aspirin-induced ulcers
- Healing of damaged oesophageal or stomach tissue (Otherwise known as oesophagitis and gastritis)
The 6-8 Week Checkpoint
Despite their effectiveness, PPIs were never intended for indefinite use without re-assessment. After the initial treatment period (typically 2-4 weeks for reflux or 6-8 weeks for ulcers), options should include:
- Reducing to the lowest effective dose
- Focusing on lifestyle and dietary measures
- Attempting to stop medication if symptoms have resolved
There are some reasons to prescribe longterm PPI
Some conditions may legitimately require extended or even lifelong PPI therapy:
- Severe erosive oesophagitis in the context of a hiatus hernia not fit for endoscopic or surgical therapy
- Barrett’s oesophagus – this condition has a low risk of turning into oesophageal cancer (the mechanism being chronic gastro-oesophageal risk)
- Ongoing need for aspirin/NSAIDs with high bleeding risk
- Zollinger-Ellison syndrome
- Other rare hyper-secretory conditions
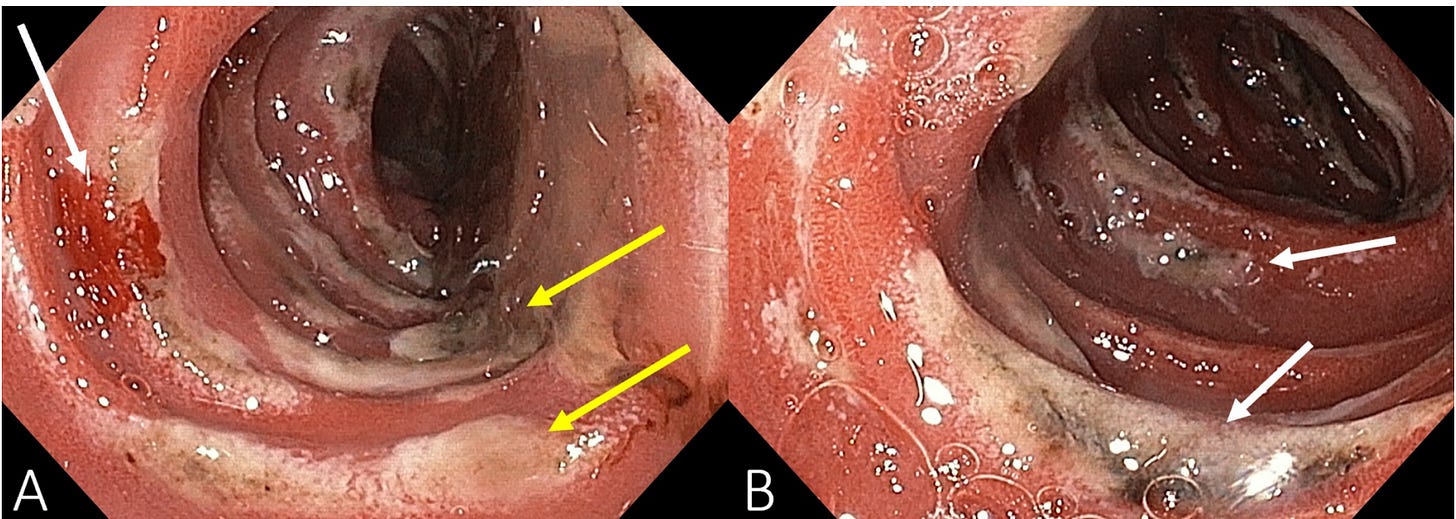
That’s the duodenum (first part of the small bowel) of someone with Zollinger-Ellison Syndrome…..I think they’re allowed the pass for longterm PPI!
Okay, so how was I “mis-sold PPI?”
I had to give some context first!
Now to answer the reason you clicked on the article in the first place…
While generally considered safe short-term, prolonged PPI therapy has been associated with several concerns:
Nutritional Deficiencies:
- Vitamin B12: Without adequate acid, B12 can’t be properly absorbed, potentially leading to neurological symptoms and anaemia. A systematic review concluded PPI users have 42% higher odds of developing B12 deficiency.
- Magnesium: PPIs may impair magnesium absorption, with studies showing nearly 3x higher risk with long-term use. Symptoms include fatigue, muscle cramps, and even cardiac issues.
Infection Risks:
- C. difficile infection: Higher stomach pH allows this dangerous bacteria to survive, while PPIs may impair immune responses. Research consistently shows higher rates in PPI users.
Clostridium dificile really close up….trust me, you don’t want to get this bug
- Small Intestinal Bacterial Overgrowth (SIBO): Studies found SIBO in 13.2% of PPI users versus only 1.8% in non-users, causing bloating, discomfort, and malabsorption.
- Other infections: Increased risk of Salmonella, Campylobacter, and other gut infections due to reduced acid barrier function.
Additional Concerns:
- Hypergastrinaemia: When acid is suppressed, your body produces more gastrin, potentially leading to cell changes and rebound acid hyper-secretion when stopping PPIs. This is why when stopping PPIs, patients may experience worsening symptoms. I explain this to patients as the “rebound reflux phenomenon”
- Bone health: Some studies suggest increased fracture risk with long-term use. The mechanism of action may be due to limited calcium absorption.
- Drug interactions: PPIs can affect absorption and metabolism of other medications
Finding Balance
PPIs are an important therapeutic advance for acid-related disorders.
However, their effectiveness has led to potential overuse in some cases.
For most people, the best approach includes:
- Periodic re-assessment of whether continued therapy is necessary
- Using the lowest effective dose
- Considering “step-down” approaches when appropriate
- Awareness and monitoring of potential side effects]
I always counsel my patients to come off their PPI. I explain the rebound reflux phenomenon as your body gets used to producing stomach acid again. The stomach has gone months, sometimes years to reduced acid production…therefore it may be a little sensitive as you come off the medication. Good news is, this phenomenon does get better over time.
If you’re currently taking a PPI, don’t stop without consulting your healthcare provider. The risks of untreated acid-related conditions can be serious, and the risk-benefit analysis must be personalised to your specific situation.
By understanding both the benefits and potential concerns of PPI therapy, you can make more informed decisions about your digestive health in partnership with your healthcare provider.
Struggling with digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
Enjoying these articles – Join my newsletter, The Gut Group: https://drhussenbux.substack.com/
References
- Prosapio JG, Sankar P, Jialal I. Physiology, Gastrin. 2023 Apr 6. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 30521243.
- Arnold R et al. Antral gastrin-producing G-cells and somatostatin-producing D-cells in different states of gastric acid secretion. Gut. 1982 Apr;23(4):285-91.
- Schubert ML. Regulation of gastric acid secretion. Curr Opin Gastroenterol. 1999 Nov;15(6):457-62.
- Liu Y et al. Gastrin (G) cells and somatostatin (D) cells in patients with dyspeptic symptoms: Helicobacter pylori associated and non-associated gastritis. J Clin Pathol. 2005 Sep;58(9):927-31
- https://www.ncbi.nlm.nih.gov/books/NBK535425/
- Kinoshita Y, Ishimura N, Ishihara S. Advantages and Disadvantages of Long-term Proton Pump Inhibitor Use. J Neurogastroenterol Motil. 2018 Apr 30;24(2):182-196.
- Haastrup PF et al. When does proton pump inhibitor treatment become long term? A scoping review. BMJ Open Gastroenterol. 2021 Feb;8(1)
- Choudhury A et al. Vitamin B12 deficiency and use of proton pump inhibitors: a systematic review and meta-analysis. Expert Rev Gastroenterol Hepatol. 2023 May;17(5):479-487
- Gommers LMM et al. Mechanisms of proton pump inhibitor-induced hypomagnesemia. Acta Physiol (Oxf). 2022 Aug;235(4)
- Patil R, Blankenship L. Proton Pump Inhibitors and Clostridium Difficile Infection: Are We Propagating an Already Rapidly Growing Healthcare Problem? Gastroenterology Res. 2013 Oct;6(5):171-173
- Revaiah PC et al. Risk of small intestinal bacterial overgrowth in patients receiving proton pump inhibitors versus proton pump inhibitors plus prokinetics. JGH Open. 2018 Apr 2;2(2):47-53
- Lehault WB, Hughes DM. Review of the Long-Term Effects of Proton Pump Inhibitors. Fed Pract. 2017 Feb;34(2):19-23
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.